Impact of comorbidity in elderly prostate cancer patients treated with brachytherapy
Introduction
Comorbidity is an important consideration in oncology practice, particularly among older patients. One of the most extensively studied instruments for measuring comorbidity was Charlson comorbidity index (CCI) (1).
In a variety of common cancers, including prostate cancer, increasing comorbidity was associated with a lower likelihood of receiving potentially curative therapy, a shorter overall survival (OS), and a greater likelihood of dying from other causes (2-6). However, elderly patients are an extremely heterogeneous population as regards comorbidity: subjects can vary from very fit to not being able to live independently due to comorbidities. Thus, unlike advanced age, clinicians may be offering a radical tratment, as brachytherapy, in a selected series of patients with low-intemediate risk disease. Dispite the lack of randomized studies and only elderly population-based studies, some institutional case series showed brachytherapy to produce excellent biochemical control (b-DFS) in elderly patients with localized prostate cancer compared with alternative curative treatments (7-10). Similar survival outcomes were showed comparing patients aged >60 years than younger with clinically localized prostate cancer and treated with brachytherapy (11,12).
The aim of our study was to evaluate the impact of comorbidity on toxicity profiles and outcomes in a series of elderly patients who underwent low-dose rate brachytherapy (LDR-BT) with 125I seeds implant.
Patients and methods
Patients characteristics
Patients aged more than 65 years and treated with LDR-BT as monotherapy, were selected for this analysis. LDR-BT was offered to patients with clinically localized prostate cancer: low-risk [T1-T2a; Gleason score (GS) ≤6; prostate specific antigen (PSA) <10 ng/mL] and intermediate-risk (T2b-T2c or GS=7; PSA=10-20 ng/mL). Risk groups were defined according to National Comprehensive Cancer Network (NCCN). Clinical stage was based on the 2002 International Union Against Cancer (UICC) (13,14).
A PSA relapse was defined according to the Phoenix definition (PSA nadir+2 ng/mL) (15). Karnofsky performance status (KPS) ≥70 and life expectancy longer than 5 years were eligible criteria for our study.
All patients underwent blood tests, including PSA level, digital rectal examination, computed tomography (CT) scan of the pelvis, bone scan, transrectal ultrasonography with multiple (≥12) needle biopsy cores of the prostate to stage disease.
Follow-up was performed every 3 months in the first year, and every 6 months in the following years. At each follow-up, PSA level was assesed and acute and late toxicity was scored using Radiotherapy Oncology Group (RTOG) toxicity scale (16).
Brachytherapy tecnique
The brachytherapy procedure was performed using a transrectal ultrasound-guided (TRUS) approach, with planned total dose of 145 Gy, according to the protocol of the American Association of Physicist in Medicine (APPM-TG 43) (17).
For each patients, a transrectal ultrasound was performed 2 weeks before the implantation date to estimate the number of radioactive sources to order and implant into prostate.
After spinal anaesthesia, the seeds implant was run with intraoperative transrectal guidance (images at 5-mm were acquired). The treatment planning was performed using the planning system (TPS) Vari Seed 8.0 (Varian Medical System, Palo Alto, CA, USA). The prostate and the organs at risk were contoured according to ESTRO guidelines (urethra, rectum and penile bulb); the dose constraints used for treatment plan evaluation were 217 Gy to 0.1 cc of the urethra and 145 Gy to 0.3 cc of the anterior rectal wall (18).
A mean of 78 seeds (range, 46-135 seeds) were implanted, with the activity of 0.400 mCi (19). Seven weeks after the implantation, a CT scan was performed for each patient to compare the planned dose distribution and the effective dose received by prostate and other organs at risk.
Charlson comorbidity index (CCI)
Comorbidity data were obtained from medical reports using age-adjusted Charlson comorbidity index (a-CCI). The Charlson score takes into account the presence of 19 diseases weighted on the basis of their association with mortality. A Charlson sum is calculated according to the number of morbidities affecting an individual. For each morbidity, a number of points are allocated and the sum of these points gives an overall score. This sum can be used in conjunction with the patient’s age as the Charlson score to calculate a probability of survival.
A malignant solid tumor is one of clinical condition associated to CCI score, in example for patient without other comorbidities, malignancy was scored with a point of 2 or 6 for metastatic desease, thus we arbitrarily decided to not considered prosate cancer as a morbidity in a-CCI calculating, firstly because all patients of our series were affected by prostate cancer and second to obtain a more homogeneous evaluation of other comorbidities in the fianl calculation of overall score.
For each patients, CCI-aged adjusted score was computed, defining two comorbidity levels: ≤3 (low-moderate) and >3 (high).
Statistical analysis
The follow-up period was calculated from the end of brachytherapy. Analysis was performed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). Survival curves were obtained with Kaplan-Meier method. Log-rank test was used to evaluate influence of comorbidity on OS. We used a cut-off point of 75 years, whereby the patients were subdivided into age ≤75 years and age ≥75 years. P<0.05 was considered statistically significant. Fisher exact test was used to determine association between age-adjusted comorbidity and acute toxicity.
Results
Patients
From June 2003 to October 2009, a total of 92 elderly patients with localized prostate underwent low-dose rate 125I brachytherapy implant at the Department of Radiation Oncology, IRCCS-CROB. The median age of patients was 75 years (range, 65-87 years). Low-risk disease occurred in 57 patients (62%) and intermediate-risk disease in 35 patients (38%). The clinical characteristics of patients are reported in Table 1. The median follow-up time was 56 months (range, 24-103 months).
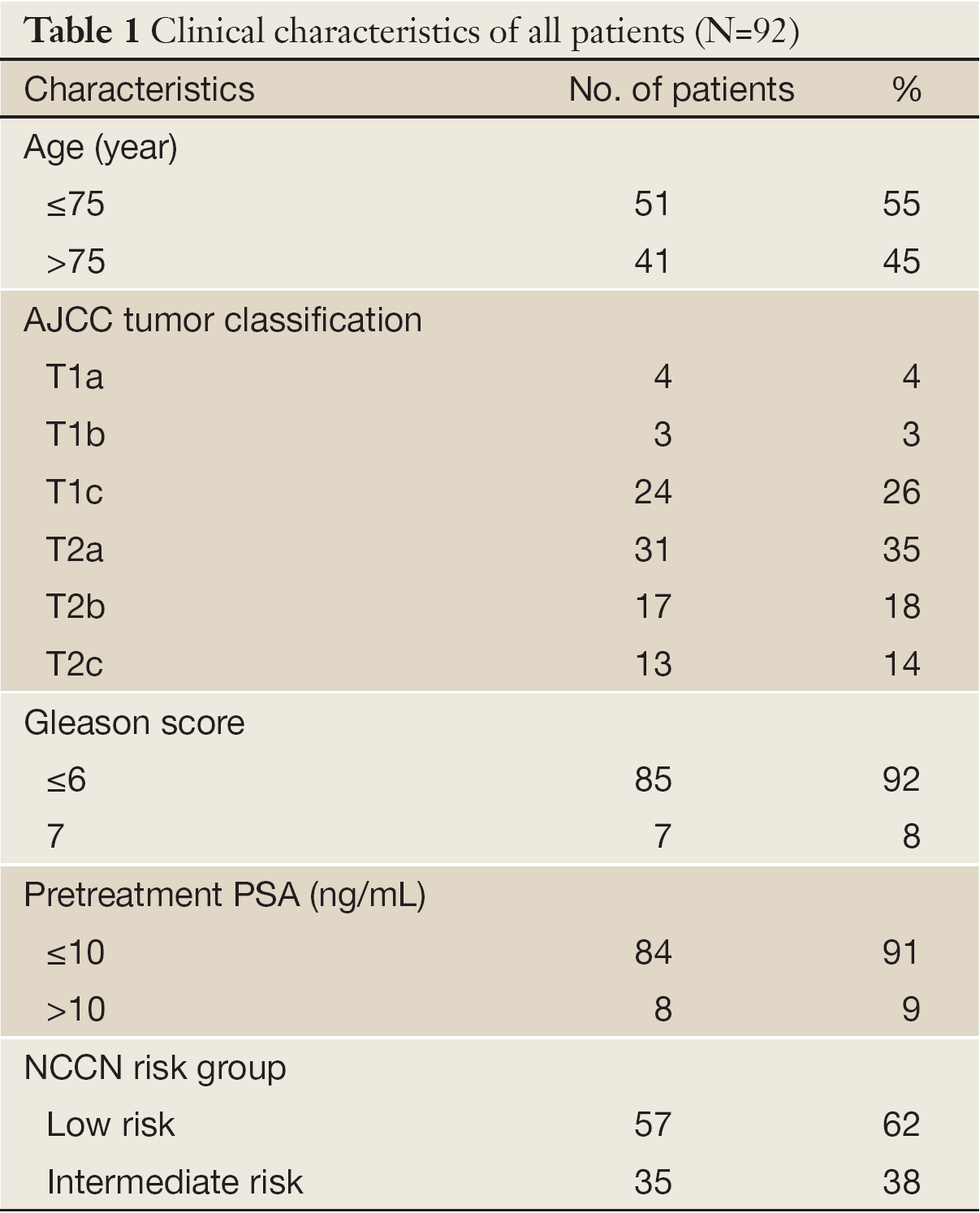
Full Table
At the time of statistical analysis, 80 patients (87%) were alive without disease, and only 4 patients (4%) were alive with disease (half of these patients had an age of greater than 75 years). There were 8 deaths (9%) over the period of follow-up, including 5 deaths from other causes and only 1 patient (age: 85 years) died for prostate cancer 72 months after brachytherapy implantation. Among this group, 6 patients were ≥75 years old and 2 patients were <75 years old.
a-CCI
The a-CCI score was calculate to be ≤3 in 47 patients (51%) and >3 in 45 patients (49%). In our series, all died patients had a-CCI ≥3. Descriptive characteristics of a-CCI score are shown in Table 2.
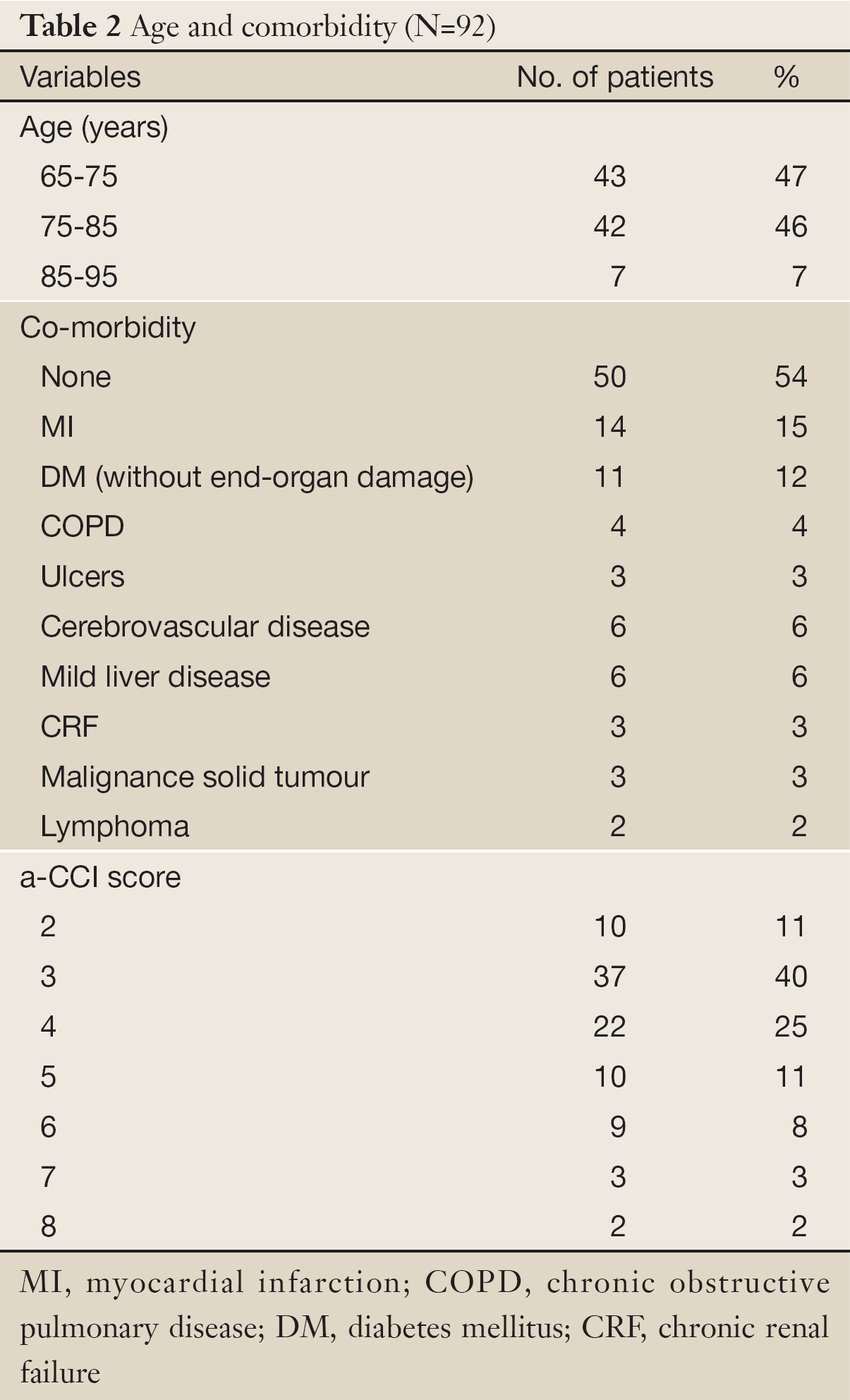
Full Table
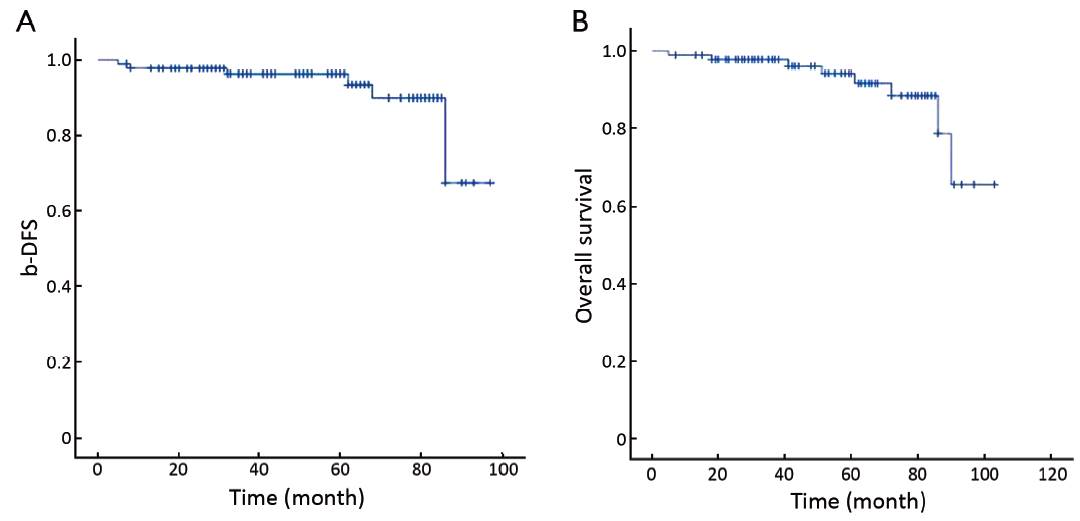
OS and biochemical disease-free survival
Biochemical recurrence occurred in 7 patients (8%) while 85 patients (92%) were free from biochemical failure. The median time to PSA failure was 27 months (range, 8-40 months). The actuarial 5-year b-DFS and OS were 92.4% and 91.3% respectively (Figure 1A,B).
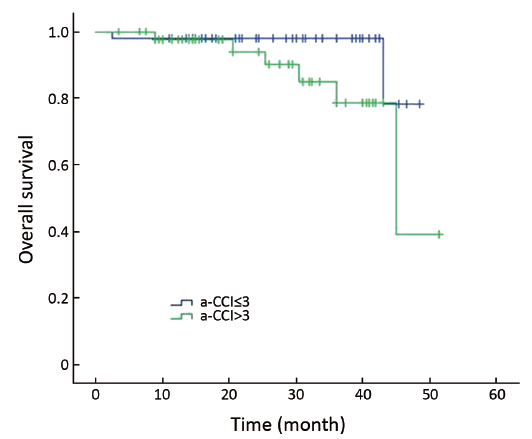
Survival analyses of non-prostate cancer mortality across Charlson groups revealed no statistical significance between two groups of patients, showing an actuarial 5-year OS of 95.7% for patients with lower-moderate comorbidity (a-Charlson score ≤3) and 5-year OS of 86.7% for those with most significant comorbidity (a-Charlson score >3) (P=0.08) (Figure 2).
Toxicity
About toxicity profile: 24 patients (26%) experienced grade-2 (G2) acute genitourinary (GU) toxicity consisting in a frequency of urination less than one hour and dysuria requiring local anesthetic drugs. Only 4 patients (4%) experienced late grade-3 (G3) GU toxicity, because of obstructive symptoms requiring transurethral resection of prostate (TURP) in 3 patients (3%) and catheterization for longer than 2 weeks in 1 patient (1%). There was no acute G3 gastrointestinal (GI) toxicity.
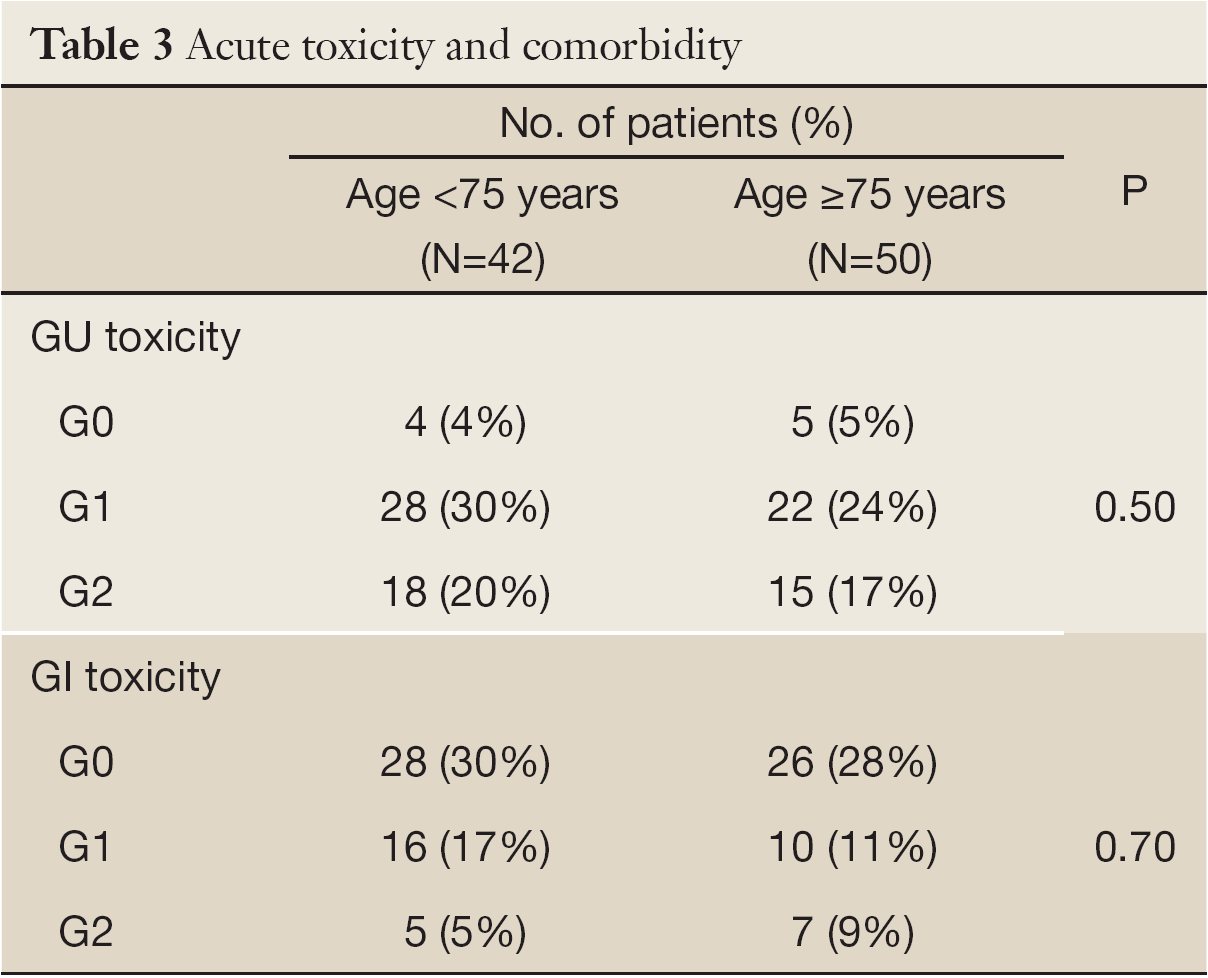
A pure nonparametric correlation analysis between acute toxicity and a-CCI was also performed using Fisher exact test, which was tailed on two groups of patients adjusted for a-CCI (≤3; >3). About acute toxicity (GU and GI), the difference between two groups was not statistically significant (P=0.50 and P=0.70 respectively) (Table 3).
Full Table
Discussion
The optimal treatment choice for clinically localized prostate cancer is controversial particularly in elderly men with presumed multiple concomitant medical morbidities. In a treatment decision making, age at diagnosis is an important determinant of therapy as remaining life expectancy, tumor grade, and comorbidity. Generally active surveillance is appropriate for men with very low risk prostate cancer when life expectancy <20 years or men with low risk disease with life expectancy <10 years (20). Literature data showed equivalent outcome, comparing radical prostatectomy, external beam radiotherapy and brachytherapy as monotherapy in clinically localized prostate cancer patients (8-21,22). However, excellent outcomes were reported in some institutional case series about elderly patients with localized prostate cancer treated with LDR-BT (23,24). In literature, there were limited data on prognostic value of comorbidity. The impact of comorbidity on survival outcomes (using Charlson score) was reported both with conservative management and with active treatment for patients with prostate cancer (25,26).
Several studies reported a clear association between comorbidity and mortality in men with prostate cancer, but others didn’t find any association (27,28). In a retrospective analysis on 107 patients aged ≥75 years, received radical external beam radiotherapy for prostate cancer, Fiorica et al. reported an acceptable rate of toxicity and a better survival for patients with mild comorbidities or good performance status (29). Neider et al. in a largely unselected cancer prostate population, including also high-risk patients, treated with radical prostatectomy or external beam radiotherapy or with endocrine treatment alone, showed a statistically significant correlation between high comorbidity and early death (30). The aim of our study was to evaluate the impact of comorbidity on survival outcomes and toxicity profiles in a series of elderly patients who underwent LDR-BT with 125I seeds implant.
However, it’s difficult to compare existing studies due to: different study design (samples, treatments), the lack of wide use of a standard comorbidity assessment and various comorbidity tools used. It’s not clear whether comorbidities can influence the acute and late toxicities due to an active treatment.
We found only one study reported urinary, bowel and erectile morbidity in unselected population-based sample of older men affected by prostate cancer who underwent brachytherapy alone, with none survival outomes evaluation. With respect to explanatory variables (demografic variables, treatment variables, tumor related variables, risk factor for complications), age and higher CCI were associated to major urinary and bowel complications (31).
We examined 92 patients to evaluate the role of comorbidity in treatment outcomes: survival and toxicity. None correlation between toxicity and comorbidity was found in our study, perhaps because our simple was “fit” to treatment with a KPS ≥70 and not had major comorbidities; furthermore in the a-CCI score calculation, each decade of age over 40, contributes 1 point to the risk index score, which is added to the score from CCI. Thus, since over half of our patients (54%) had an age ≥75 years, probably, age had more impact on the a-CCI score than the medical comorbidity conditions.
About OS, we found no significant difference between two comorbidity groups, although the 5-year OS was shorter in patients with a-CCI >3 with respect to those with a-CCI ≤3. These data, probably, depend on the small simple size and the follow-up period.
Many different tools are available for the assessment of comorbidity but only few studies examined the performance of different comorbidity measures in prostate cancer setting, thus the optimal comorbidity index for clinical use remains unclear (32,33).
A radical approach is a safe and effective strategy, in elderly cancer patients (34,35). Our data suggest that comorbidity does not affect compliance to treatment and even results in terms of OS and b-DFS. As reported in a previous work, we believe that LDR-BRT could have a great role in elderly men treatment choice because it is a safety and efficacy treatment (36).
Although several studies have investigated the value of CCI to predict outcomes after radical prostatectomy, further studies are needed to investigate about ideal comorbidity assesment tool in elderly prostate cancer patients treated with brachytherapy (37-39).
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. [PubMed]
- Yan Y, Carvalhal GF, Catalona WJ, et al. Primary treatment choices for men with clinically localized prostate carcinoma detected by screening. Cancer 2000;88:1122-30. [PubMed]
- Alibhai SM, Krahn MD, Cohen MM, et al. Is there age bias in the treatment of localized prostate carcinoma? Cancer 2004;100:72-81. [PubMed]
- Litwin MS, Greenfield S, Elkin EP, et al. Assessment of prognosis with the total illness burden index for prostate cancer: aiding clinicians in treatment choice. Cancer 2007;109:1777-83. [PubMed]
- Albertsen PC, Fryback DG, Storer BE, et al. The impact of co-morbidity on life expectancy among men with localized prostate cancer. J Urol 1996;156:127-32. [PubMed]
- Newschaffer CJ, Otani K, McDonald MK, et al. Causes of death in elderly prostate cancer patients and in a comparison nonprostate cancer cohort. J Natl Cancer Inst 2000;92:613-21. [PubMed]
- Pickles T, Keyes M, Morris WJ. Brachytherapy or conformal external radiotherapy for prostate cancer: a single-institution matched-pair analysis. Int J Radiat Oncol Biol Phys 2010;76:43-9. [PubMed]
- Kupelian PA, Potters L, Khuntia D, et al. Radical prostatectomy, external beam radiotherapy <72 Gy, external beam radiotherapy > or =72 Gy, permanent seed implantation, or combined seeds/external beam radiotherapy for stage T1-T2 prostate cancer. Int J Radiat Oncol Biol Phys 2004;58:25-33. [PubMed]
- Colberg JW, Decker RH, Khan AM, et al. Surgery versus implant for early prostate cancer: results from a single institution, 1992-2005. Cancer J 2007;13:229-32. [PubMed]
- Morris WJ, Keyes M, Palma D, et al. Population-based study of biochemical and survival outcomes after permanent 125I brachytherapy for low- and intermediate-risk prostate cancer. Urology 2009;73:860-5; discussion 865-7. [PubMed]
- Hinnen KA, Roeloffzen EM, Battermann JJ, et al. Survival after prostate brachytherapy in patients aged 60 years and younger. BJU Int 2011;107:1906-11. [PubMed]
- Stone NN. Survival after prostate brachytherapy in patients aged 60 years and younger. BJU Int 2011;107:1911. [PubMed]
- D’Amico AV, Whittington R, Malkowicz SB, et al. Pretreatment nomogram for prostate-specific antigen recurrence after radical prostatectomy or external-beam radiation therapy for clinically localized prostate cancer. J Clin Oncol 1999;17:168-72. [PubMed]
- Sobin LH, Witteking CH. eds. TNM Classification of Malignant Tumors. 6th ed. New York: Wiley-Liss, 2002.
- Roach M 3rd, Hanks G, Thames H Jr, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 2006;65:965-74. [PubMed]
- Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys 1995;31:1341-6. [PubMed]
- Nath R, Anderson LL, Luxton G, et al. Dosimetry of interstitial brachytherapy sources: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. American Association of Physicists in Medicine. Med Phys 1995;22:209-34. [PubMed]
- Salembier C, Lavagnini P, Nickers P, et al. Tumour and target volumes in permanent prostate brachytherapy: a supplement to the ESTRO/EAU/EORTC recommendations on prostate brachytherapy. Radiother Oncol 2007;83:3-10. [PubMed]
- Pinkawa M, Asadpour B, Gagel B, et al. Evaluation of source displacement and dose--volume changes after permanent prostate brachytherapy with stranded seeds. Radiother Oncol 2007;84:190-6. [PubMed]
- NCCN Guidelines Version 1. 2012 Prostate Cancer. Available online: http://www.nccn.org/professionals/physicians_ gls/f _guidelines. asp# prostate
- D’Amico AV, Whittington R, Kaplan I, et al. Equivalent biochemical failure-free survival after external beam radiation therapy or radical prostatectomy in patients with a pretreatment prostate specific antigen of > 4-20 ng/ml. Int J Radiat Oncol Biol Phys 1997;37:1053-8. [PubMed]
- Keyser D, Kupelian PA, Zippe CD, et al. Stage T1-2 prostate cancer with pretreatment prostate-specific antigen level < or = 10 ng/ml: radiation therapy or surgery? Int J Radiat Oncol Biol Phys 1997;38:723-9. [PubMed]
- Morris WJ, Keyes M, Palma D, et al. Population-based study of biochemical and survival outcomes after permanent 125I brachytherapy for low- and intermediate-risk prostate cancer. Urology 2009;73:860-5; discussion 865-7. [PubMed]
- Hinnen KA, Roeloffzen EM, Battermann JJ, et al. Survival after prostate brachytherapy in patients aged 60 years and younger. BJU Int 2011;107:1906-11. [PubMed]
- Albertsen PC, Hanley JA, Fine J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 2005;293:2095-101. [PubMed]
- Tewari A, Johnson CC, Divine G, et al. Long-term survival probability in men with clinically localized prostate cancer: a case-control, propensity modeling study stratified by race, age, treatment and comorbidities. J Urol 2004;171:1513-9. [PubMed]
- Daskivich TJ, Chamie K, Kwan L, et al. Comorbidity and competing risks for mortality in men with prostate cancer. Cancer 2011;117:4642-50. [PubMed]
- Hall HI, Satariano WA, Thompson T, et al. Initial treatment for prostate carcinoma in relation to comorbidity and symptoms. Cancer 2002;95:2308-15. [PubMed]
- Fiorica F, Berretta M, Colosimo C, et al. Safety and efficacy of radiotherapy treatment in elderly patients with localized prostate cancer: a retrospective analysis. Arch Gerontol Geriatr 2010;51:277-82. [PubMed]
- Nieder C, Dalhaug A, Pawinski A, et al. Comorbidity, use of common medications, and risk of early death in patients with localized or locally advanced prostate cancer. ScientificWorldJournal 2011;11:1178-86. [PubMed]
- Chen AB, D’Amico AV, Neville BA, et al. Patient and treatment factors associated with complications after prostate brachytherapy. J Clin Oncol 2006;24:5298-304. [PubMed]
- Alibhai SM, Leach M, Tomlinson GA, et al. Is there an optimal comorbidity index for prostate cancer? Cancer 2008;112:1043-50. [PubMed]
- Singh R, O’Brien TS. Comorbidity assessment in localized prostate cancer: a review of currently available techniques. Eur Urol 2004;46:28-41; discussion 41. [PubMed]
- Fiorentino A, Caivano R, Chiumento C, et al. Comorbidity assessment and adjuvant radiochemotherapy in elderly affected by glioblastoma. Med Oncol 2012;29:3467-71. [PubMed]
- Chun SH, Lee JE, Park MH, et al. Gemcitabine Plus Platinum Combination Chemotherapy for Elderly Patients with Advanced Non-small Cell Lung Cancer: A Retrospective Analysis. Cancer Res Treat 2011;43:217-24. [PubMed]
- Chiumento C, Fiorentino A, Caivano R, et al. Low-dose rate brachytherapy of the prostate in elderly patients. Radiol Med 2012. [Epub ahead of print] [PubMed]
- Froehner M, Koch R, Litz R, et al. Which conditions contributing to the Charlson score predict survival after radical prostatectomy? J Urol 2004;171:697-9. [PubMed]
- Froehner M, Koch R, Litz RJ, et al. Feasibility and limitations of comorbidity measurement in patients undergoing radical prostatectomy. Eur Urol 2005;47:190-5; discussion 195. [PubMed]
- Kastner C, Armitage J, Kimble A, et al. The Charlson comorbidity score: a superior comorbidity assessment tool for the prostate cancer multidisciplinary meeting. Prostate Cancer Prostatic Dis 2006;9:270-4. [PubMed]