Huang’s three-step maneuver for laparoscopic spleen-preserving No. 10 lymph node dissection for advanced proximal gastric cancer
Clinical vignette
The lymph nodes (LNs) in the splenic hilar area, including the LNs along the distal splenic vessels (No. 11d) and the splenic hilum (No. 10), should be removed for normative D2 LN dissection during total gastrectomy for advanced proximal gastric cancer (1). However, spleen-preserving splenic hilar lymphadenectomy is now widely used in total gastrectomy with D2 LN dissection due to combined resection of the pancreas and spleen significantly increasing postoperative morbidity and mortality rather than improving prognosis, as well as decreasing immunological function (2-4). With the rapid development of minimally invasive surgery, the application of laparoscopic surgery for gastric cancer is gradually gaining popularity. However, due to the complexity of the splenic hilar vessels, their anatomical variation and the narrow and deep space, as well as the bleeding-prone splenic parenchyma and the difficulty to manage splenic or vascular bleeding at the splenic hilum, the procedure remains challenging and technically demanding procedure for the performance of laparoscopic pancreas- and spleen-preserving splenic hilar LN dissection. Based on our experiences with laparoscopic pancreas- and spleen-preserving splenic hilum LN dissection in more than 350 gastric cancer patients, we gradually explored a set of procedural operation steps called “Huang’s three-step maneuver”. Herein, the detailed procedure is presented.
Surgical techniques
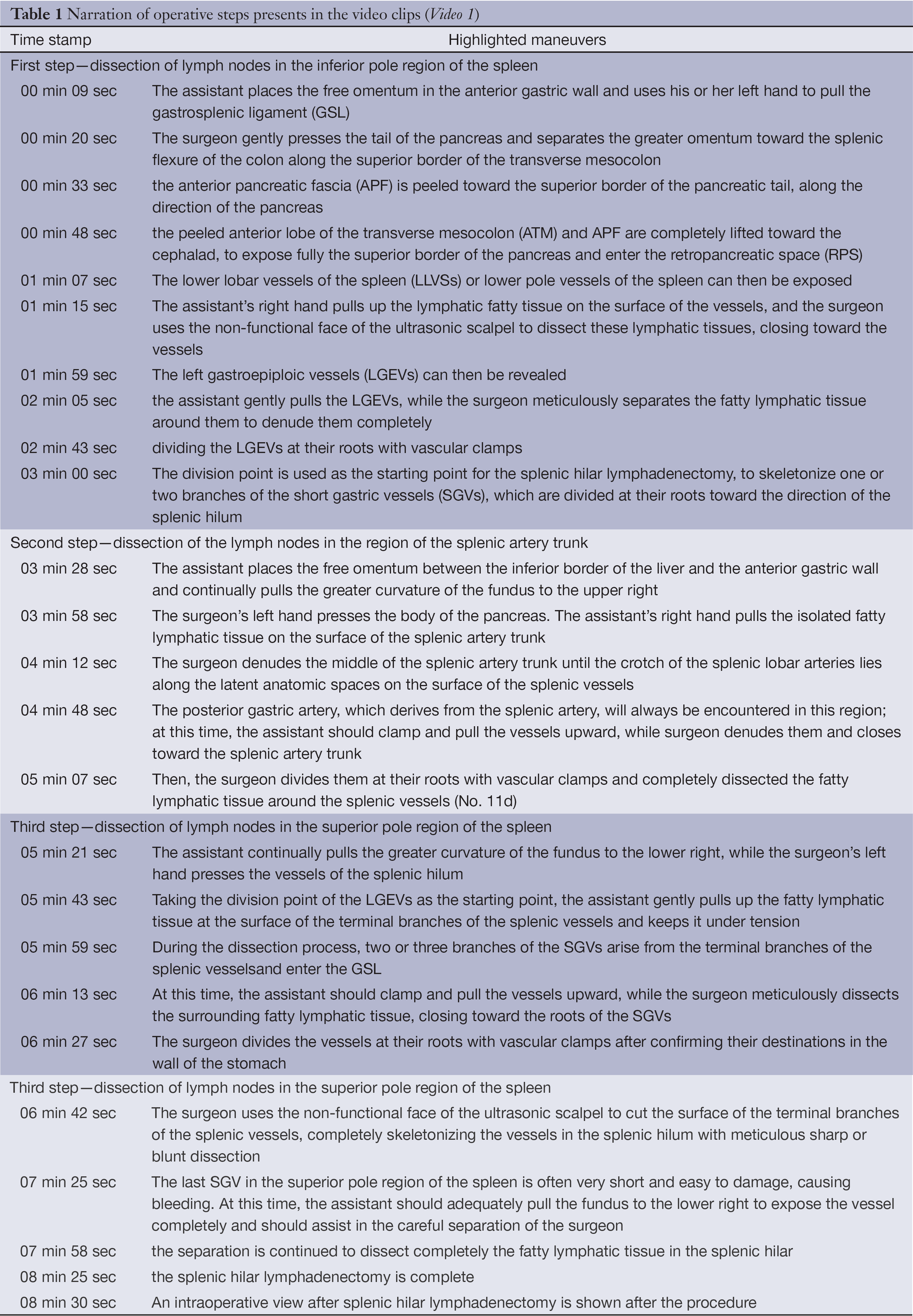
The patient was placed in the reverse Trendelenburg position with their head elevated approximately 15 to 20 degrees and tilted left-side up approximately 20 to 30 degrees. The surgeon stood between the patient’s legs, with the assistant and camera operator both on the patient’s right side. The Table 1 lists a timed narrative to help locate specific points in the procedure.
Comments
Splenic hilar lymphadenectomy is an important component in laparoscopy-assisted radical total gastrectomy for advanced proximal gastric cancer, and it is quite sophisticated and technically demanding. The surgeon should fully understand the anatomical features of the splenic hilar vessels under laparoscopic viewing, and he or she should undertake a reasonable surgical approach, as well as procedural operation steps based on vascular anatomy. We have summarized our experience, learned lessons and gradually explored this set of procedural operation steps after laparoscopic pancreas- and spleen-preserving splenic hilar LN dissection in more than 350 gastric cancer patients. We have realized in practice that a steady and tacit understanding and teamwork play important roles in this procedure. Hence, we not only provide the concrete operation steps for the surgeon, but we also provide our recommended technique of pulling and exposure for assistants. This new maneuver simplifies the complicated procedure and improves the efficiency of laparoscopic spleen-preserving splenic hilar lymphadenectomy, making it easier to master and allowing for its widespread adoption.
Acknowledgements
Sponsored by National Key Clinical Specialty Discipline Construction program of China (No. [2012] 649).
Disclosure: The authors declare no conflict of interest.
References
- Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer 2011;14:113-23. [PubMed]
- Hyung WJ, Lim JS, Song J, et al. Laparoscopic spleen-preserving splenic hilar lymph node dissection during total gastrectomy for gastric cancer. J Am Coll Surg 2008;207:e6-11. [PubMed]
- Okabe H, Obama K, Kan T, et al. Medial approach for laparoscopic total gastrectomy with splenic lymph node dissection. J Am Coll Surg 2010;211:e1-6. [PubMed]
- Sakuramoto S, Kikuchi S, Futawatari N, et al. Laparoscopy-assisted pancreas- and spleen-preserving total gastrectomy for gastric cancer as compared with open total gastrectomy. Surg Endosc 2009;23:2416-23. [PubMed]