Effect of internal iliac artery chemotherapy after transurethral resection of bladder tumor for muscle invasive bladder cancer
Introduction
Bladder cancer is one of the most commonly encountered urinary carcinoma, of which about 15-25% is muscle invasive bladder cancer (MIBC). Clinically, tumor invasion to meet or exceed the muscle of the bladder is defined as the MIBC, which has high rate of tumor recurrence and metastasis, and poor prognosis. Currently, the preferred treatment of MIBC is radical cystectomy, which can improve the survival rate of patients, and avoid local recurrence and distal metastasis. Due to surgical complications and life inconvenience resulted from urinary diversion, patients are reluctant to accept this surgical method. It is also difficult to suggest this method to the elderly patients who also have a serious system disease (1).
In recent years, with the 2-micron laser transurethral resection of bladder tumor (TUR-BT) performed, the effect of transurethral resection of bladder becomes more favorable. The resection of whole layers of bladder becomes safer. With the internal iliac artery chemotherapy and intravesical chemotherapy, those patients may have the tumor treated and at the same time the bladder can be safely preserved.
We summarized the clinical data of 62 patients treated in Peking University Cancer Hospital and Beijing Xuanwu Hospital, who were diagnosed as the MIBC, from February 2007 to April 2014, in order to analyze the feasibility and safety of this method of bladder preservation in MIBC patients.
Materials and methods
Patient selection
Sixty-two patients with MIBC who underwent operation with bladder preservation from February 2007 to April 2014 in Peking University Cancer Hospital and Beijing Xuanwu Hospital, with or without internal iliac artery chemotherapy, were analyzed. All the patients received cystoscopy biopsy and were confirmed to have a bladder transitional cell carcinoma pathologically and graded tumor. Magnetic resonance imaging (MRI) examinations were performed to confirm the diagnosis of MIBC.
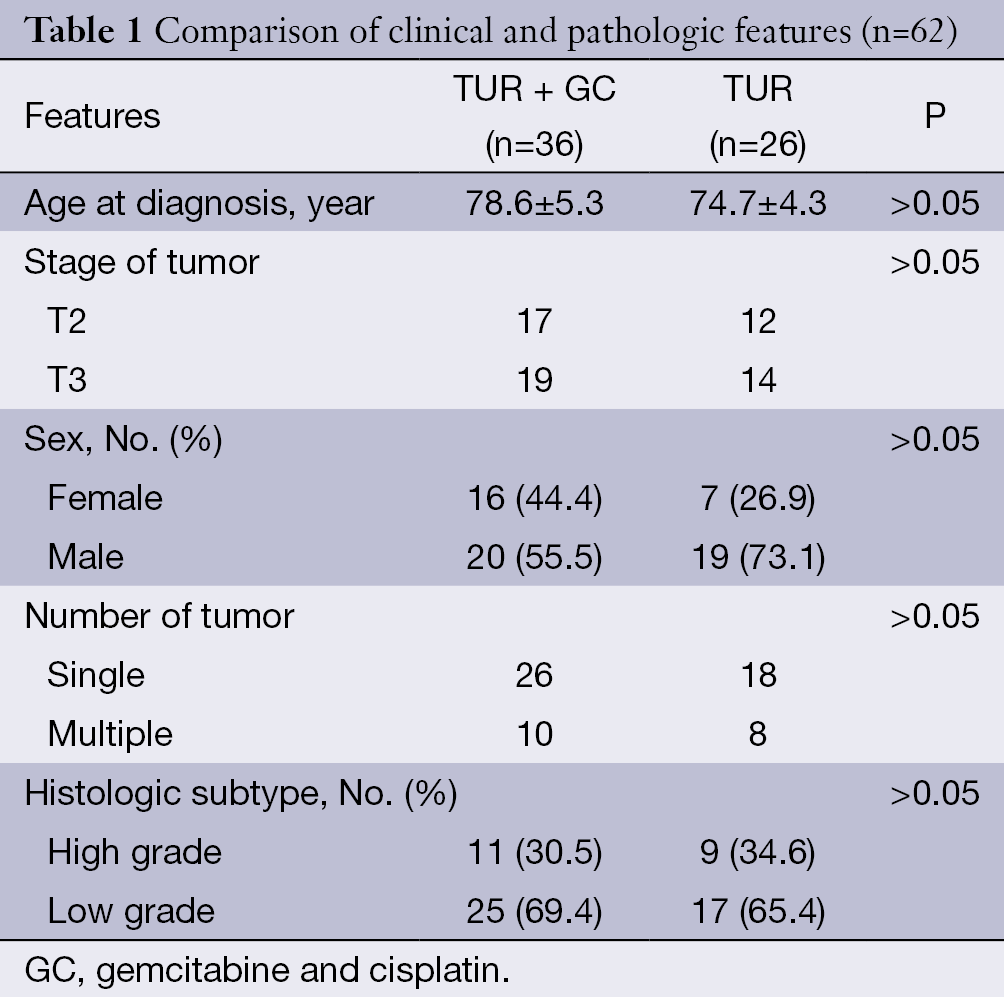
In this study, according to their underlying diseases and patients’ will, 36 of 62 cases underwent TUR-BT therapy combined with internal iliac artery chemotherapy [chemotherapy regimen is gemcitabine and cisplatin (GC), GC regimen]. Afterwards, we analyzed the outcome of TUR + GC group and TUR group. Both of the groups received intravasical instillation of anti-cancer chemical agent as routine. Clinical and pathologic features for the 62 patients are depicted in Table 1. Between the TUR + GC group and TUR only groups, there were no differences in age at diagnosis, tumor stage, gender, tumor number and histologic subtypes.
Full table
Surgical treatment
RevoLix 2-micron continuous wave laser was produced by the German LISA medical laser surgery system. Laser wavelength is 2.013 micron, and energy transmitted via 550 µm optical fiber. Transurethral resection endoscopy, Fr26 (12°) was made by Karl Storz. Patients were put in litho trim position with intravenous anesthesia, and laser equipment power was adjusted to 15-30 W. During operation, we used low-pressure continuous saline bladder instillation, and cut the tumor around 1 cm from tumor margin by laser cutting and vaporization. Cutting depth may reach deep muscle layer of the bladder or outer membrane. At the end of resection, biopsy should be performed at the base of the tumor. Continuous irrigation of the bladder with distilled water should be done after surgery. Re-TUR-BT should be carried out within 4-6 weeks if basal pathology was positive.
Intravesical instillation chemotherapy
Instant instillation chemotherapy was performed within 24 h immediately after surgery. Chemotherapy regimen was epirubicin 50 mg or pirarubicin 30 mg, dissolved in 50 mL saline, and retained for 30 min during intravesical instillation. This chemotherapy was performed once a week for 10 weeks, and then once a month for 1-2 years (2).
Internal iliac artery chemotherapy
In TUR + GC group, arterial infusion chemotherapy was performed at 1 month after operation for the first time, then monthly for two times, later once every 3 months in the first year, and then every 6 months in the second year. The GC chemotherapy regimen was gemcitabine 600-800 mg/m2 plus cisplatin 50 mg/m2. Guide catheter got through the left or right femoral artery, and then into the iliac arteries by Seldinger technique. After injection of chemotherapy drugs, full hydration and symptomatic treatment were adopted after arterial infusion chemotherapy (3,4).
Clinical follow-up
Patients’ complete blood count (CBC), urinalysis, and liver and kidney function analyses were monitored daily within 1 week after arterial infusion chemotherapy. At the time of hospitalization for arterial chemotherapy, bladder enhanced MRI, urinary tract enhanced computed tomography urography (CTU), and cystoscopy with random multi-point bladder biopsy were also arranged to determine whether there was tumor recurrence. For local recurrence, they would receive 2-micron laser vaporization for further treatment. Overall follow-up was arranged every 3 months including lung checking, bone scans, and liver examination. If repeat recurrence presented, the patient would be recommended to receive radical cystectomy therapy or systemic chemotherapy. Meanwhile, the overall survival (OS) and disease-free survival (DFS) were analyzed by Kaplan-Meier analysis with SAS software (version 9.1) (SAS Institute Inc., USA).
Results
Patients’ characteristics and postoperative follow-up
The patients were composed of 39 males and 23 females, of which 34 patients were over 80 years old at diagnosis, 21 cases 75-80 years old, and seven cases 70-75 years old. The main clinical symptom of the patients was asymptomatic hematuria. For the concern of age, underlying diseases and anxiety on postoperative complications of radical cystectomy, these patients underwent 2-micron laser TUR-BT and intravesical instillation therapy. In these 62 patients, 55 cases had hypertension, 51 cases with electrocardiogram (ECG) ST-T changes, 27 cases with previous history of myocardial infarction, six patients with cardiac pacemaker, 33 cases with pulmonary ventilatory reserve obstacles, and 22 patients with other underlying diseases such as diabetes. All patients received scheduled treatment and follow-up. The clinical and pathologic features had no statistically significant difference. They were followed-up for 26-102 months, mean 58.4±3.1 months. In TUR + GC group (n=36), 28 cases (77.8%) survived without recurrence and metastasis, and eight cases (22.2%) appeared recurrence from the 2nd to 26th months, who underwent 2-micron laser TUR-BT treatment and restarted chemotherapy programs then. Two patients of them underwent radical cystectomy and urinary diversion for the positive tumor base with high grade urothelial carcinoma and recurrence for two times. Twenty-eight patients survived during the follow-up period, three patients died of bladder tumor progression, two died of cardiopulmonary causes, two died of other underlying diseases, and one died of small cell lung cancer with biopsy. In TUR group (n=26), 11 cases (42.3%) survived without recurrence and metastasis, and 15 cases (57.7%) showed recurrence from 4th to 46th months, five of which underwent radical cystectomy. Metastases to the lung and retroperitoneal lymph nodes were detected in three cases, one of which died for lesions in the lung 8 months after diagnosis, and the other two received intravenous chemotherapy. Three patients died of local advanced bladder cancer lesions, and one died of his cerebrovascular disease.
Side effects of chemotherapy
In the TUR + GC group, no serious local adverse reactions and systemic side effects were observed during arterial infusion chemotherapy. Seventeen cases complained of mild postoperative gastrointestinal reactions such as nausea and abdominal discomfort and then disappeared 3-7 d after symptomatic treatment. Six patients had transient peripheral blood leukocyte reduction, and after colony stimulating factor treatment, they got back to normal and became stable within 1 week. One patient suffered with alopecia, and no obvious cardiac or kidney dysfunction was observed.
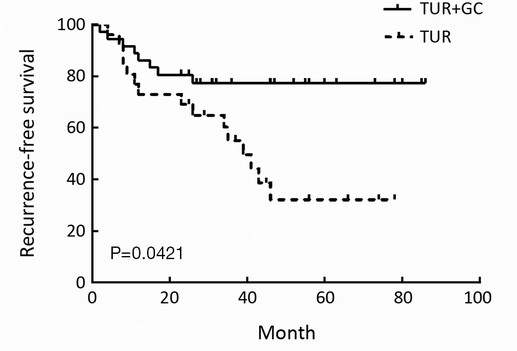
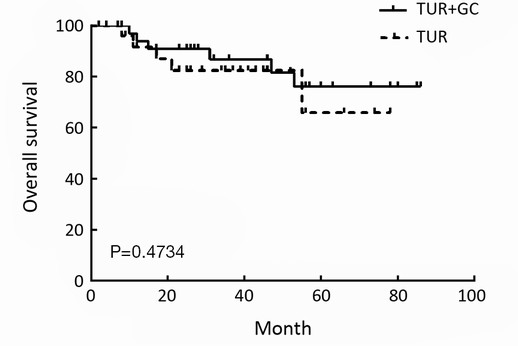
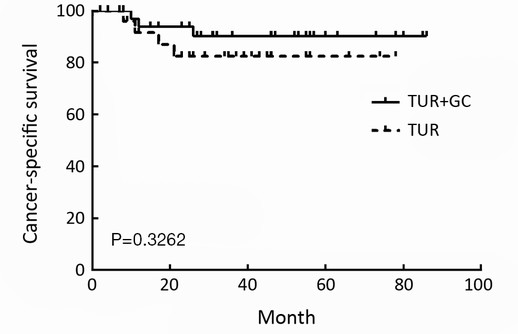
Survival rate analysis
Recurrence-free survival (RFS) at 2-year for TUR + GC group and TUR group were 77.8% and 53.8%, respectively. Bladder preserved rate (BPR) at 2-year for TUR + GC group and TUR group were 94.4% had 80.8%. DFS rates at 1-year for TUR + GC group and TUR group were 83.3% and 61.5%, and 77.8% and 53.8% for the 2nd year. These results had statistically significant difference between two groups (P<0.05). Cancer-specific survival (CSS) rates at 2-year for TUR + GC group and TUR group were 94.4% and 84.6%. OS rates at 2-year for TUR + GC group and TUR group were 88.9% and 92.3%. These results showed no statistically significant difference between two groups (Table 2, Figures 1,2,3).
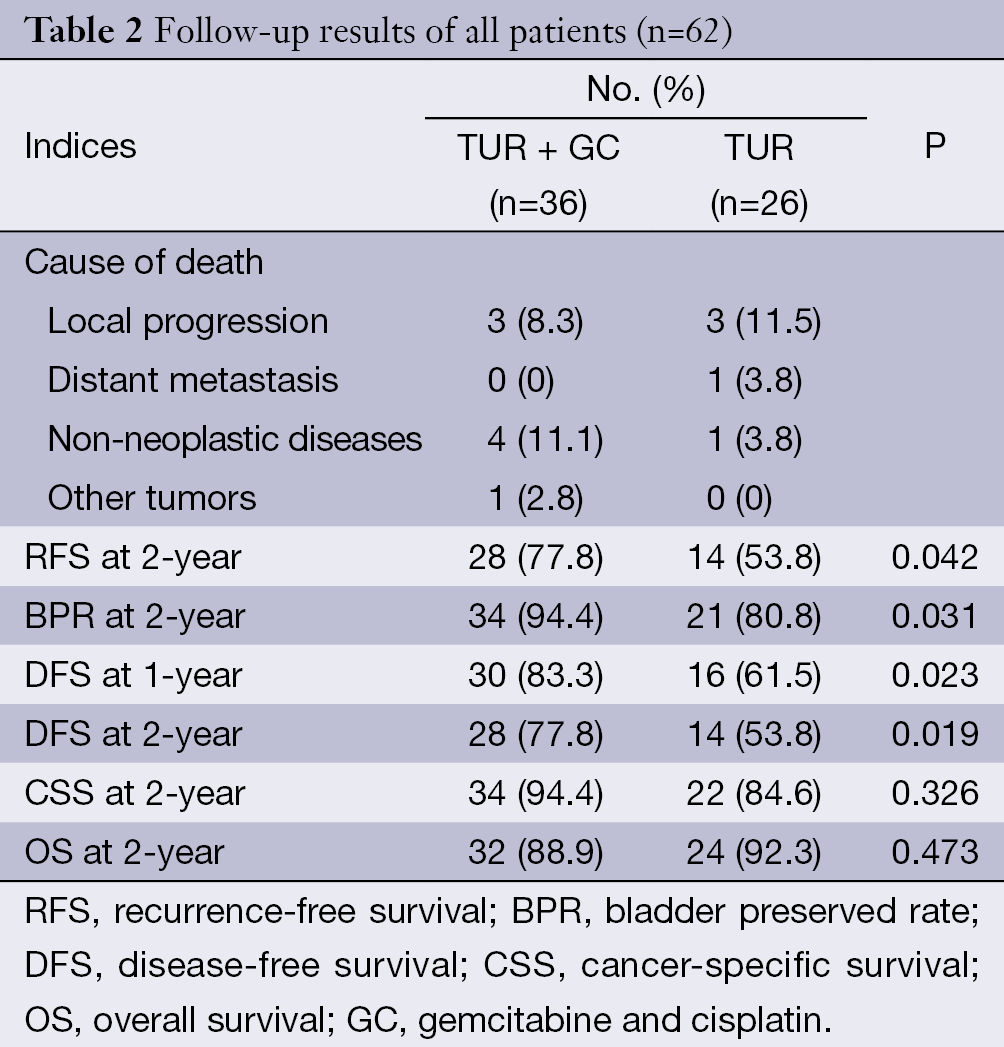
Full table
Discussion
In this study, we compared the outcome of TUR-BT and intravesical instillation therapy combined with or without internal iliac artery chemotherapy for MIBC. OS and CSS were similar between two groups. However, the RFS, BPR, and DFS were superior in TUR + GC group.
Radical cystectomy is still the gold standard treatment for MIBC currently. However, due to surgical trauma, high complication incidence and poor quality of post operation living quality, some patients are reluctant to accept this treatment method. Furthermore, considering the patient’s age and underlying diseases, it is difficult to carry out in some patients. Therefore, plenty of research has been devoted in the treatment of MIBC, aiming to preserve bladder function.
TUR-BT is the main treatment for non-MIBC (5). It can remove the tumor, also may provide information of clinical stage and pathological grade to guide further treatment. Residual tumor rate was 33-76% after TUR-BT (6,7), 15-61% of patients will show recurrence within 1 year, and 31-78% recurrence occurs within 5 years after TUR-BT (8). It is associated with postoperative residual tumor or muscle invasion.
In order to achieve the aim of bladder preservation, TUR surgery combined with systemic chemotherapy was planned. Patients’ complete remission (CR) rate was 72.0-85.7%, 5-year CSS was 64.0-75.7%, and OS was 52.0-67.7% (9-11). However, because of the characteristics of blood circulation of the chemotherapy drugs, the systemic side effects of chemotherapy were obvious. It is often more difficult for patients to tolerate this treatment.
The main blood supply of bladder cancer lesion is from the iliac arteries, so internal iliac artery infusion chemotherapy drugs can increase the drug concentration of tumor blood vessels, which provides less systemic reactions, and the efficacy is up to 24 times higher than intravenous administration. Intra-arterial chemotherapy will be one of the main regional treatments for MIBC. In other articles, the CR rate of internal iliac artery chemotherapy was 76.0-93%, the bladder preservation rate was 83.9-89.7%, and the 5-year survival rate was 61.3% (12-15). Data showed that 20-30% of the MIBC patients after TUR-BT can still have superficial bladder cancer. Intravesical instillation chemotherapy drugs have been shown to be effective for prevention and treatment of bladder cancer for local recurrence (16). In summary, internal iliac artery infusion chemotherapy and intravesical instillation chemotherapy can reduce the rate of tumor recurrence and improve survival and prognosis after TUR surgery.
Furthermore, we also think that 2-micron laser TUR-BT has further advantages. Laser can converse into heat rapidly, and diathermy of energy is only 0.13 mm, which may help controlling the scope and depth of cutting, so the cutting borderline may be fine and smooth, especially for tumor around the ureteral orifice. No obturator nerve reflection happens, which can make cutting deeper, even the whole layer of bladder, thus it helps to reduce tumor recurrence, and less bleeding as well (17). This provoked more research in preservation of bladder with MIBC (18-20).
The limitation of this study is that the number of cases still needs to be enlarged, and there are selection biases of treatment. A randomized controlled trial is needed to confirm the optimal management of patients with MIBC who still hope to reserve the bladder.
Conclusions
In our research, we observed that TUR-BT and intravesical instillation therapy combined with internal iliac artery chemotherapy for MIBC, which may have a better outcome at RFS, BPR and DFS than the TUR-BT treatment only, and also have the similar OS and CSS. These data suggest that for the benefit of some special MIBC patients, TUR-BT and intravesical instillation therapy combined with internal iliac artery chemotherapy may be a reasonable choice.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hussain M, Theodorescu D. Bladder cancer: bladder preservation--learning what we don’t know. Nat Rev Urol 2014;11:310-2. [PubMed]
- Chen SY, Du LD, Zhang YH. Pilot study of intravesical instillation of two new generation anthracycline antibiotics in prevention of superficial bladder cancer recurrence. Chin Med J (Engl) 2010;123:3422-6. [PubMed]
- Mantadakis E, Panagiotidis C, Delakas D, et al. Symptomatic relief of patients with advanced bladder carcinoma after regional intra-arterial chemotherapy. Anticancer Res 2003;23:5143-7. [PubMed]
- Khaled HM, Shafik HE, Zabhloul MS, et al. Gemcitabine and Cisplatin as Neoadjuvant Chemotherapy for Invasive Transitional and Squamous Cell Carcinoma of the Bladder: Effect on Survival and Bladder Preservation. Clin Genitourin Cancer 2014;12:e233-40. [PubMed]
- Wilby D, Thomas K, Ray E, et al. Bladder cancer: new TUR techniques. World J Urol 2009;27:309-12. [PubMed]
- Babjuk M, Burger M, Zigeuner R, et al. EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol 2013;64:639-53. [PubMed]
- Ali MH, Ismail IY, Eltobgy A, et al. Evaluation of second-look transurethral resection in restaging of patients with nonmuscle-invasive bladder cancer. J Endourol 2010;24:2047-50. [PubMed]
- Sylvester RJ, van der Meijden AP, Oosterlinck W, et al. Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 2006;49:466-5; discussion 475-7.
- Efstathiou JA, Spiegel DY, Shipley WU, et al. Long-term outcomes of selective bladder preservation by combined-modality therapy for invasive bladder cancer: the MGH experience. Eur Urol 2012;61:705-11. [PubMed]
- Perdonà S, Autorino R, Damiano R, et al. Bladder-sparing, combined-modality approach for muscle-invasive bladder cancer: a multi-institutional, long-term experience. Cancer 2008;112:75-83. [PubMed]
- Sabaa MA, El-Gamal OM, Abo-Elenen M, et al. Combined modality treatment with bladder preservation for muscle invasive bladder cancer. Urol Oncol 2010;28:14-20. [PubMed]
- Azuma H, Inamoto T, Takahara K, et al. The novel bladder preservation therapy BOAI-CDDP-radiation (OMC-regimen): a new treatment option for invasive bladder cancer patients with lymph node metastasis. Int J Oncol 2014;44:1895-903. [PubMed]
- Hashine K, Kusuhara Y, Miura N, et al. Bladder preservation therapy conducted by intra-arterial chemotherapy and radiotherapy for muscle invasive bladder cancer. Jpn J Clin Oncol 2009;39:381-6. [PubMed]
- Miyanaga N, Akaza H, Hinotsu S, et al. Background Variables for the Patients with Invasive Bladder Cancer Suitable for Bladder-preserving Therapy. Jpn J Clin Oncol 2007;37:852-7. [PubMed]
- Shimabukuro T, Nakamura K, Uchiyama K, et al. Angiotensin-II combined intra-arterial chemotherapy for locally advanced bladder cancer: a case series study at a single institution. Hinyokika Kiyo 2006;52:99-105. [PubMed]
- Chen X, Liao J, Chen L, et al. En bloc transurethral resection with 2-micron continuous-wave laser for primary non-muscle-invasive bladder cancer: a randomized controlled trial. World J Urol 2014. [Epub ahead of print].
- Han B, Liang S, Jing Y, et al. Organ preservation for muscle-invasive bladder cancer by preoperative intra-arterial chemotherapy and transurethral resection. Med Oncol 2014;31:912. [PubMed]
- Na SW, Yu SH, Kim KH, et al. The prognosis of patients less than 40 years with bladder cancer. J Cancer Res Ther 2014;10:710-4. [PubMed]
- Miyata Y, Nomata K, Ohba K, et al. Efficacy and safety of systemic chemotherapy and intra-arterial chemotherapy with/without radiotherapy for bladder preservation or as neo-adjuvant therapy in patients with muscle-invasive bladder cancer: A single-centre study of 163 patients. Eur J Surg Oncol 2014. [Epub ahead of print]. [PubMed]
- Devanand P, Kim SI, Choi YW, et al. Inhibition of bladder cancer invasion by Sp1-mediated BTG2 expression via inhibiting DNA methyltransferase 1. FEBS J 2014. [Epub ahead of print]. [PubMed]
