A case of small intestinal hemorrhage secondary to metastatic lung cancer in the elderly
Introduction
In patients with lung cancer, distant metastases to the brain, bone, kidney, adrenal gland, and other organs are common but metastases affecting the gastrointestinal tract are relatively rare (1). We report a case of bleeding in the small intestine, secondary to metastatic lung cancer, a very rare complication in the natural history of this cancer.
Case report
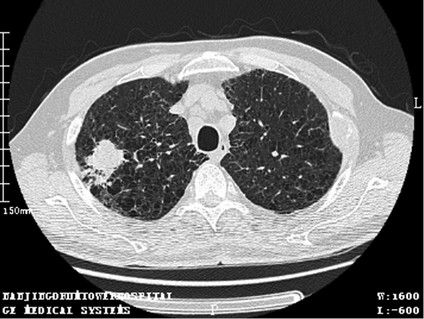
A 78-year-old male was admitted complaining of “Passing dark red blood for 4 hours”. He had a 20-year history of diabetes, as well as a smoking history of 25 cigarettes per day since the age of 18. Four months previously, he was diagnosed with lung adenocarcinoma [TXN1M1 (adrenal gland, bone, lymph node), stage IV] (Figure 1). After diagnosis, he had Alimta chemotherapy but this was terminated due to intolerance. From then on, he only took medicine to control his cough and sputum. Physical examination showed: a temperature of 36.5 °C, blood Z His consciousness was clear. His face was pale. His abdomen was soft with mild but not rebound tenderness in the left upper abdomen. The liver and spleen were untouched and there were no masses. Fluid thrill was negative. Shifting dullness was negative. Borborygmus not heard.
On admission, his blood test results were: leukocyte count 8.8×109/L, neutrophil count 75.1%, hemoglobin 63 g/L, and platelets 122×109/L. We gave the patient fasting acid suppression, somatostatin hemostasis, a blood transfusion and intravenous nutrition. After 2 hours, the patient began to feel nauseous, and hematemesis was approximately 60 mL with blood clots. Blood pressure dropped to 90/50 mmHg. Bedside gastroscopy showed that there was no bleeding in the stomach. Superior mesenteric artery angiography digital subtraction angiogram (DSA) showed a superior mesenteric artery jejunal hemorrhage, but DSA cannot provide any further information. So we conducted an emergency laparotomy under general anesthesia. A 2.5 cm × 2.5 cm mass was found in the jejunum, about 3 cm from the ligament of Treitz. Jejunum wedge resection was carried out and bleeding was controlled. Two months after the operation, the patient died from severe pulmonary infection.
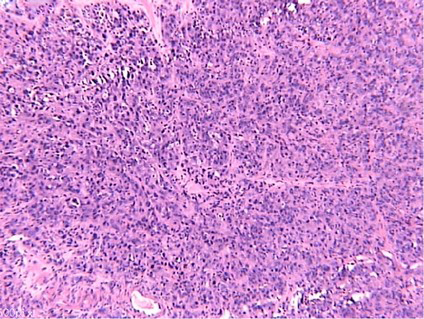
Pathology results showed a –2.2 × 1.8 × 0.8 cm submucosal nodule was in the intestinal wall. Microscopic findings confirmed the invasion of tumor cell growth, cell atypia, and mitoses (Figure 2). Immunohistochemical staining showed that the cancer cells expressed TTF1 (+), villin (–), CDX2 (–), CK7 (+), CK20 (–). These findings confirmed a diagnosis of small intestinal malignant tumor, and poorly differentiated metastatic carcinoma.
Discussion
In lung cancer, metastasis to the gastrointestinal tract is rare, ranging from 0.2% to 1.7% in reported studies (2,3). However, autopsy reports state the prevalence of gastrointestinal metastasis in lung cancer is 4.7% to 14% (4). Most gastrointestinal metastasis has no obvious symptoms, and consequently they are very difficult to detect.
There is a male predominance over females in the development of symptomatic small bowel lung cancer metastasis in the literature; the mean age in patients with small bowel lung cancer metastasis was 64.5 years (5). The most common clinical manifestations were perforation (59%), followed by obstruction (29%), while hemorrhage is rare (10%) (6).
Small bowel metastasis has been shown to occur with all histological subtypes of lung cancer. Garwood et al. (5), found adenocarcinoma and squamous cell carcinoma to be the most common histological subtypes, which correlated exactly with the most common histological subtypes of primary lung tumors.
Immunohistochemistry has a special role in the determination of metastatic tumor primary lesion. Our patient presented with immunohistochemistry staining of TTF-1 (+), CK7 (+), CK20 (–), villin (–) and CDX2 (–). The expression pattern of CK7, CK20 and villin in different carcinomas is helpful for determining the origin of some metastatic adenocarcinomas, and minimizing the range of origin of metastatic adenocarcinomas. Weihua et al. (7), found that CK7+/CK20– /villin– in 392 samples of tumor tissue there was a high positive rate for: breast invasive lobular carcinoma (100%), pulmonary adenocarcinoma (95%), and ovarian serous adenocarcinoma (70%). Then use corresponding organ-specificity antibody, such as the gastrointestinal tract with CDX2, lung cancer and thyroid cancer with TTF-1, to finalize the tumor organ source.
The general route for metastasis from lung cancer to the gastrointestinal tract has been suggested to be hematogenous metastasis via the spinal veins or lymphogenous metastasis from the mediastinum through the retroperitoneum and mesentery (8). In our patient, the metastasis was thought to be hematogenous because no obvious metastasis to the mesentery or dissemination to the retroperitoneum was seen during surgery, and a solitary nodule was found in the resected small intestine specimen.
Once intestinal bleeding, obstruction or perforation occurs following lung cancer metastasis, surgical resection of metastatic lesions can be performed. This is conducive to the improvement of abdominal symptoms. However, because of the primary disease, the overall prognosis is very poor, with a mean survival time of 2 to 4 months.
In conclusion, if elderly male patients with lung cancer present with painless gastrointestinal bleeding, gastrointestinal metastasis should be considered. Immunohistochemical pathological examination is the gold standard for diagnosis. Local operation resection can improve symptoms.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Steinhart AH, Cohen LB, Hegele R, et al. Upper gastrointestinal bleeding due to superior mesenteric artery to duodenum fistula: rare complication of metastatic lung carcinoma. Am J Gastroenterol 1991;86:771-4. [PubMed]
- Yoshimoto A, Kasahara K, Kawashima A. Gastrointestinal metastases from primary lung cancer. Eur J Cancer 2006;42:3157-60. [PubMed]
- Rossi G, Marchioni A, Romagnani E, et al. Primary lung cancer presenting with gastrointestinal tract involvement: clinicopathologic and immunohistochemical features in a series of 18 consecutive cases. J Thorac Oncol 2007;2:115-20. [PubMed]
- Lermite E, Pessaux P, Du Plessis R, et al. Small bowel metastasis from primary lung carcinoma. Gastroenterol Clin Biol 2004;28:307-9. [PubMed]
- Garwood RA, Sawyer MD, Ledesma EJ, et al. A case and review of bowel perforation secondary to metastatic lung cancer. Am Surg 2005;71:110-6. [PubMed]
- Hillenbrand A, Sträter J, Henne-Bruns D. Frequency, symptoms and outcome of intestinal metastases of bronchopulmonary cancer. Case report and review of the literature. Int Semin Surg Oncol 2005;2:13. [PubMed]
- Weihua L, Xiaoge Z, Yanning Z. Combined application of CK7, CK20 and villin and its values in judging the origin of metastatic carcinoma. J Diag Pathol 2008;15:275-78.
- Yamada H, Akahane T, Horiuchi A, et al. A case of lung squamous cell carcinoma with metastases to the duodenum and small intestine. Int Surg 2011;96:176-81. [PubMed]