Anatomical variation of infra-pyloric artery origination: A prospective multicenter observational study (IPA-Origin)
Introduction
Gastric cancer is one of the most common malignant tumors worldwide and infra-pyloric artery (IPA) is an important anatomical landmark for its treatment (1,2). The IPA is the predominant artery to the pyloric antrum (3). For early gastric cancer, the IPA must be preserved in the pylorus-preserving gastrectomy (PPG) to maintain the blood supply and normal function of pylorus (2,4-6). In the 15th Japanese gastric cancer classification guideline, the infra-pyloric (No. 6) lymph node (LN) can be divided into 3 sections: the 6a, 6v, and 6i LN sections; and the 6i section is defined as LNs along with IPA (7,8). Thus, a thorough understanding of the anatomical variation of the IPA is very important (9).
The importance of the IPA was brought to attention just in recent years, and most studies were based on angiography and autopsy with limited sample size. Due to the small size of the vessel, the anatomy of the IPA is still poorly understood. Sawai et al. evaluated the pyloric vascular anatomy of 210 celiac angiograms and showed that the IPA originated from gastroduodenal artery (GDA) in 63.8% of all patients and originated from other arteries in the other 36.2% of patients (23.8% from pancreaticoduodenal arcade and 12.4% from right gastroepiploic artery) (4). In a study based on 20 autopsies by Shen et al., the IPA likewise mainly originated from GDA (51.6%) and right gastroepiploic artery (RGEA, 29.0%) (10). However, in a more recent study by Haruta et al. based on 156 surgical dissection and specimens, most of the IPAs originated from the anterior superior pancreaticoduodenal artery (ASPDA, 64.2%) or the root of the RGEA (23.1%), and only a small portion originated from the GDA (12.7%) (11). Thus, the anatomical variation of the IPA origination remains controversial and the data sample of existed evidence is too limited to clarify the variation. We did this “IPA-Origin” study to clarify the anatomical variation of the IPA origination.
Materials and methods
Study design
We did this prospective, multicenter, open-label, observational study at gastric surgery departments in 34 hospitals in China. Gastric cancer patients aged 18 years or older and scheduled to undergo elective total or distal gastrectomy were asked to participate in the study before surgery and to sign the informed consent form. We excluded patients whose No. 6 LNs were clinically enlarged and the IPA dissection was inappropriate for cancer surgery, and those who received surgery but without the IPA dissected, photographed, or video-recorded.
The study protocol was approved by the Institutional Review Board of Medical Ethics Committee of Peking University Cancer Hospital, and by the review boards of each study center before the initiation of patient enrollment. All participants gave written informed consent. A data monitoring board was constituted before the start of the study for data collection, quality control and progress monitoring. The board consisted of two surgeons and one statistician. In order to minimize the selection and reporting bias that surgeons may avoid to report unfavorable cases after surgery, the basic information and surgical plan of the patients were required to be reported to the board at least one day before surgery. The progress of the study was reported to all investigators every week by the data monitoring board.
Procedure and clinicopathologic evaluation
Dissecting of the IPA and exposing the origination point were required during the surgery. The intraoperative photographs or surgical video clips that could show the origination of the IPA must be taken or recorded. For patients whose IPA was identified as absence, a surgical video clip was required for review. After the surgery, the photographs or the surgical video clips with the IPA origination marked by the investigators would be sent to the data monitoring board. For the cases that the IPA origination could not be identified clearly, the photographs or the video clips would be sent to all investigators and be discussed through an instant-messaging software to clarify the origination.
The gastrectomy type was defined as total gastrectomy or distal gastrectomy. The operation approach was recorded as open surgery, laparoscopic-assisted surgery or totally laparoscopic surgery. The clinical TNM stage of the tumor was evaluated clinically according to the 7th American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) gastric cancer staging system (12). The location of tumor was defined according to the Japanese classification of gastric carcinoma as esophagogastric junction, upper third, middle third, and lower third of the stomach (13). The geographic area was defined as the area that the patient was born and was divided into 7 regions according to the Chinese geographical division as follows: East China, North China, South China, Central China, Northwestern China, Northeastern China, and Southeastern China.
Outcomes
The primary outcome of the study was the origination of the IPA, defined as the upstream artery where the root of the IPA was located. If there was only one IPA identified, the origination of the IPA would be recorded as the GDA, the RGEA, the ASPDA, or the other artery else. If multiple IPAs were identified, originations of each IPA would be recorded. If the IPA was not identified, the origination would be defined as absence.
Statistical analysis
We postulated that the IPA mainly originated from the GDA. On the basis of the results of the study by Sawai et al., we calculated that 372 patients would be needed to produce a two-sided 95% confidence interval (95% CI) with a width equal to 10% when the sample proportion is 64%. We aimed for a total of 409 patients to correct for an estimated 10% loss to follow-up.
We analyzed differences between groups of the IPA origination with analysis of variance (ANOVA) for continuous variables, χ2 tests and Fisher’s tests for categorical variables. Normal distribution of data was tested and confirmed by Kolmogorov-Smirnov test. A two-sided P-value of less than 0.05 was regarded as statistically significant. All values are expressed in the following manner unless otherwise stated: n (%) or median (interquartile range, IQR). We did statistical analysis with IBM SPSS Statistics (Version 20.0; IBM Corp., New York, USA). This study is registered at Clinicaltrials.gov (No. NCT03071237).
Results
Patient characteristics
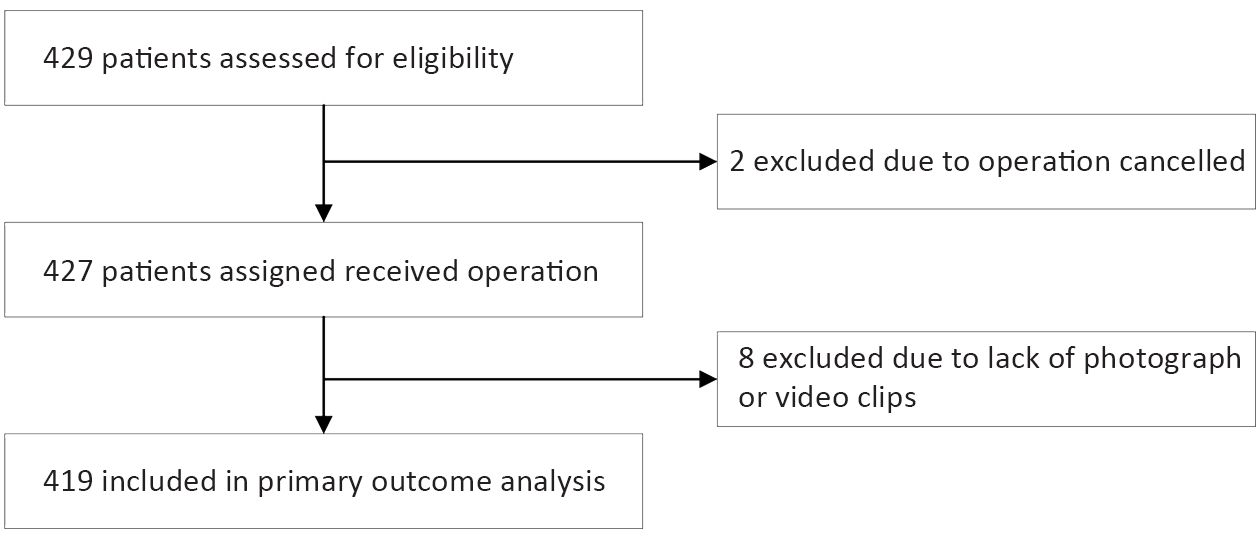
Figure 1 shows the study profile. Between May 8 and July 31, 2017, we considered and assessed the eligibility of 429 patients for the study. Four hundred and nineteen (97.7%) patients had the IPA dissected and recorded through photograph or video during gastrectomy and were included in the primary outcome analysis (Figure 1). The location of centers and numbers of patients enrolled in each center are shown in Supplementary Table S1.

Full table
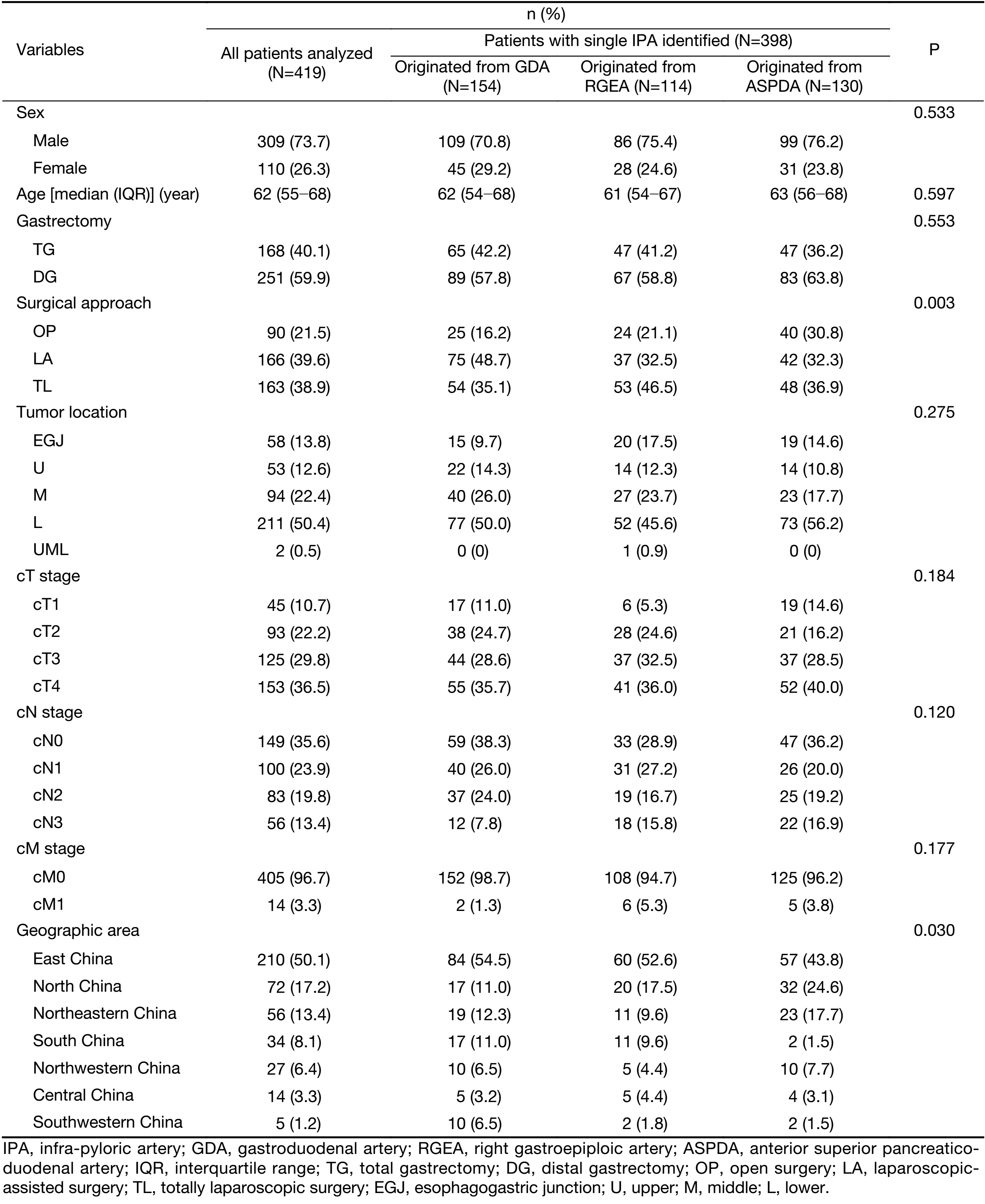
Baseline characteristics are shown in Table 1. The median age of all patients was 62 (IQR, 55−68) years old and 73.7% of the patients were male. Most patients received laparoscopic surgery (78.5%) and distal gastrectomy (59.9%). Most of the tumors were located in the middle or lower third of the stomach (72.8%) and locally advanced gastric cancer was the main part (85.9%). Most patients (80.7%) were from East China, North China and Northeastern China.
Full table
IPA origination and its relationship with clinicopathological characteristics
Of 419 patients analyzed, single IPA origination was identified in 398 patients (95.0%, 95% CI: 92.9%−97.1%), including GDA in 154 patients (36.8%, 95% CI: 32.2%−41.4%), ASPDA in 130 patients (31.0%, 95% CI: 26.6%−35.4%), and RGEA in 114 patients (27.2%, 95% CI: 22.9%−31.4%). Fifteen patients (3.6%, 95% CI: 1.8%−5.4%) were identified with multiple IPA origination (Table 2) and 6 patients (1.4%, 95% CI: 0.3%−2.5%) were identified as IPA absence. There was no statistically significant difference in clinicopathological factors among patients with single origination, multiple originations and IPA absence (Supplementary Table S2).

Full table

Full table
Of 398 patients with single IPA identified, the clinicopathological factors were compared among patients with different originations (Table 1). The differences in the distribution of surgical approach (P=0.003) and geographic area (P=0.030) were statistically significant. No difference was shown in sex, age, gastrectomy type, tumor location, and clinical T, N and M stage.
Among the 15 patients with multiple IPAs, there were 13 patients with 2 IPAs, 1 patient with 3 IPAs and 1 patient with 4 IPAs (Table 2). Thirteen of the 15 patients had at least one IPA originated from the RGEA.
Patients without IPA identified were compared with those with IPA identified, and no statistically significant difference was observed.
Discussion
Our findings show that the IPA originates from GDA (36.8%), ASPDA (31.0%) and RGEA (27.2%) in similar proportions. A small proportion of patients are with multiple IPAs or with IPA unable to be identified.
The IPA is a small artery first described by Rossi et al. in 1904 and is the main blood supply for the pylorus (3,14,15). For early gastric cancer that is suitable for PPG, the IPA must be preserved to maintain the blood supply of pylorus and the dissection of the IPA is the key technique for the surgery (2,4,5). For patients whose IPA is absent or cannot be clearly identified and preserved, PPG cannot be performed. According to the 15th Japanese classification of gastric cancer, the No. 6 LNs can be divided into 3 subgroups: the 6a, 6v, and 6i LNs based on the study of Shinohara et al. (7). Among these subgroups, the 6i LNs lie along with the IPA. However, whether the lymphatic drainage of 6i LNs would be affected by the anatomical variation is still not clear.
Studies evaluating the origin of the IPA are few and the results are obviously different. Sawai et al. reported that the proportions of the IPA originated from the GDA, RGEA, and ASPDA were 63.8%, 12.4%, and 21.4% based on 210 celiac angiograms (4). And there were 2.4% of IPAs originated from posterior superior pancreaticoduodenal arcade and no IPA absence was observed. According to the study by Shen et al. based on 20 autopsies, the IPAs were identified in all cases and 51.6% of the IPA originated from the GDA, 29.0% from the RGEA, and 19.4% from the ASPDA (10). In Shen’s study, two IPAs were observed in 55% of all cases and all the IPAs that originated from ASPDA were located closely to the root of the ASPDAs. In a more recent study by Haruta et al. based on 156 laparoscopic intraoperative dissection and postoperative specimen processing, in 73.7% of the patients, the IPA was located intraoperatively, and in the remaining 26.3% of the patients, the IPA was detected postoperatively in specimens (11). In Haruta’s study, 64.2% of the IPA originated from the ASPDA, 23.1% from the RGEA, and 12.7% from the GDA, which is obviously different from studies of Sawai and Shen. In our study, the IPA is located intraoperatively in 98.6% of the patients, and 36.8% singly originated from the GDA, 31.0% from the ASPDA, and 27.2% from the RGEA. There are 3.6% of the patients identified with multiple IPAs and 86.7% of the patients have at least one IPA originating from the RGEA.
There are several possible reasons for the variety in the proportions of the IPA origination reported in different studies. The first possible explanation is genetic factors which may be reflected by the geographic area of the patients. By far, the proportions reported by studies in Japan and China appear to be different. In our study, the distribution of the IPA origination shows statistically significant difference in different geographical regions.
Additionally, the potential reason for this inconsistency may be the difference in the methods used to identify the IPA. Sawai’ study and Shen’s study identified the IPA with angiogram or autopsy, which can detect the IPA of small size or with rare origination such as poster superior pancreaticoduodenenal arcade. Haruta’s study and our study identified the IPA mainly by intraoperative IPA dissection. If the IPA is too small or originate insidiously, it may not be identified intraoperatively. This part of patients should be paid with more attention if PPG is planned. Furthermore, surgical approach may be associated with capacity of effective detection of the IPA intraoperatively. We found the distribution of IPA origination differed by the surgical approaches performed. Particularly, the proportion that the IPA originated from the GDA was lower in open surgery compared to laparoscopic surgery. One potential explanation for this phenomenon is as following. The Haruta’s study showed that the length of the IPA from pyloric ring to proximal branch is the shortest if the IPA originated from the GDA (9.0 mm from the GDA vs. 21.8 mm from the ASPDA vs. 20.6 mm from the RGEA, P<0.01). In laparoscopic surgery, as opposed to open surgery, the surgical field is digitally enlarged and the identification of short vessels can be more accurate. The shorter length of the IPA may lead to a higher risk of intraoperatively unconscious dividing of the vessel. From this point, the PPG is more suitable to be performed by laparoscopic surgery than by open surgery.
Another reason that may affect the identification of the IPA is the learning curve of the surgeons who dissected the IPA during the surgery. The dissection of small vessels such as the IPA is an advanced technique and requires more adept skills than that of large vessels. For surgeons with limited experience, small IPA may be undetected intraoperatively and reported as an absence. In our study, the top two centers regarding the enrollment numbers recruited 26.5% of all analyzed patients. Among patients in these two centers, the IPA mainly originated from the ASPDA, followed by the RGEA and the GDA (41.4%, 38.7%, 15.3%, respectively, P<0.001). These proportions are closer to the result of Haruta’s study which was likewise conducted in a large hospital.
The main limitation of our study is that the patients participated is not a consecutive cohort and selection or reporting bias may exist. In order to minimize the bias, the enrollment of the patients was arranged before surgery and patients whose surgery were cancelled or had no photographs or videos recorded are excluded from the analysis. This helps to control the bias. Secondly, some surgeons in our study are lack of experience of the IPA dissection, which may result in the inaccuracy of the IPA dissection. From this point, the result of our study may not be able to fully prove the IPA distribution difference by regions due to the imbalance of patient distribution and surgeon experience by geographical regions. However, this is a better reflection of the real clinical practice setting, as compared with angiograms and autopsies. Another limitation is that most patients (80.7%) were from East China, North China and Northeastern China, and this distribution imbalance reflects that the study sample may be not representative enough of Chinese gastric cancer patients.
Conclusions
Our study found that the IPA originates from GDA (36.8%), ASPDA (31.0%), and RGEA (27.2%) in similar proportions. Laparoscopic surgery may be more helpful in dissection of the IPA than open surgery. To our best knowledge, this study is by far the largest study to describe the anatomical variation of the IPA and therefore can provide helpful information for studies on PPG and subgroups of the No. 6 LNs. However, the current study did not explore the association between the different origination of the IPA and its influence on PPG or lymphatic drainage of the No. 6 LNs, which needs to be further examined in the future studies.
Acknowledgements
The study is funded by the Gastric Cancer Diagnose and Treatment Project (D171100006517004, D17110700650000) of Beijing Municipal Science & Technology Commission and supported by Beijing Municipal Administration of Hospital Clinical Medicine Development of Special Funding Support (ZYLX201701).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chen W, Zheng R, Zuo T, et al. National cancer incidence and mortality in China, 2012. Chin J Cancer Res 2016;28:1–11. [PubMed] DOI:10.3978/j.issn.1000-9604.2016.02.08
- Zhang J, Cao L, Wang Z, et al. Pylorus- and vagus-nerve-preserving partial gastrectomy (D2 dissection). Chin J Cancer Res 2013;25:457–9. [PubMed] DOI:10.3978/j.issn.1000-9604.2013.08.08
- Vandamme JP, Bonte J. The blood supply of the stomach. Acta Anat (Basel) 1988;131:89–96. [PubMed] DOI:10.1159/000146493
- Sawai K, Takahashi T, Fujioka T, et al. Pylorus-preserving gastrectomy with radical lymph node dissection based on anatomical variations of the infrapyloric artery. Am J Surg 1995;170:285–8. [PubMed] DOI:10.1016/S0002-9610(05)80015-7
- Maki T, Shiratori T, Hatafuku T, et al. Pylorus-preserving gastrectomy as an improved operation for gastric ulcer. Surgery 1967;61:838–45. [PubMed] DOI:10.1016/S0002-9610(05)80015-7
- Shimada A, Takeuchi H, Ono T, et al. Pylorus-preserving surgery based on the sentinel node concept in early gastric cancer. Ann Surg Oncol 2016;23:4247–52. [PubMed] DOI:10.1245/s10434-016-5358-1
- Shinohara H, Kurahashi Y, Kanaya S, et al. Topographic anatomy and laparoscopic technique for dissection of no. 6 infrapyloric lymph nodes in gastric cancer surgery. Gastric Cancer 2013;16:615–20. [PubMed] DOI:10.1007/s10120-012-0229-3
- Mizuno A, Shinohara H, Haruta S, et al. Lymphadenectomy along the infrapyloric artery may be dispensable when performing pylorus-preserving gastrectomy for early middle-third gastric cancer. Gastric Cancer 2017;20:543–7. [PubMed] DOI:10.1007/s10120-016-0632-2
- Kim M, Son SY, Cui LH, et al. Real-time vessel navigation using indocyanine green fluorescence during robotic or laparoscopic gastrectomy for gastric cancer. J Gastric Cancer 2017;17:145–53. [PubMed] DOI:10.5230/jgc.2017.17.e17
- Shen L, Zhong Z, Tian G, et al. The observation and clinical significance of inferior pylorus artery. Zhonghua Jie Pou Yu Lin Chuang Za Zhi (in Chinese) 2006;4:223–5,228. DOI:10.3969/j.issn.1671-7163.2006.04.002
- Haruta S, Shinohara H, Ueno M, et al. Anatomical considerations of the infrapyloric artery and its associated lymph nodes during laparoscopic gastric cancer surgery. Gastric Cancer 2015;18:876–80. [PubMed] DOI:10.1007/s10120-014-0424-5
- Washington K. 7th edition of the AJCC cancer staging manual: stomach. Ann Surg Oncol 2010;17:3077–9. [PubMed] DOI:10.1245/s10434-010-1362-z
- Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer 2011;14:101–12. [PubMed] DOI:10.1007/s10120-011-0041-5
- Kuroda C, Nakamura H, Sato T, et al. Normal anatomy of the pyloric branch and its diagnostic significance in angiography. Acta Radiol Diagn (Stockh) 1982;23:479–84. [PubMed] DOI:10.1177/028418518202300507
- Rossi G, Cova E. Studio morfolgico delle arterie dello stomaco. Arch Ital Anat Embriol 1904;3:485.