Synchronous double primary lung cancer: a report of three cases
Introduction
The incidence of synchronous multiple primary lung cancers is on the rise due to improvements in computed tomography (CT) scanning and increasing use of positron emission tomography scanning and other diagnostic modalities (1). Patients with synchronous bronchogenic tumors typically present with centrally located disease that is most often reported to be of squamous cell histology (2). We report three cases of synchronous double primary lung cancer (DPLC). All diagnoses were based on CT findings, results of bronchoscopic examinations, and histological study of the biopsy specimens. Our analysis of the patients’ risk factors, tumor sites, and histological classifications may enhance the understanding of DPLC.
Case presentation (Figures 1-3)
Case 1
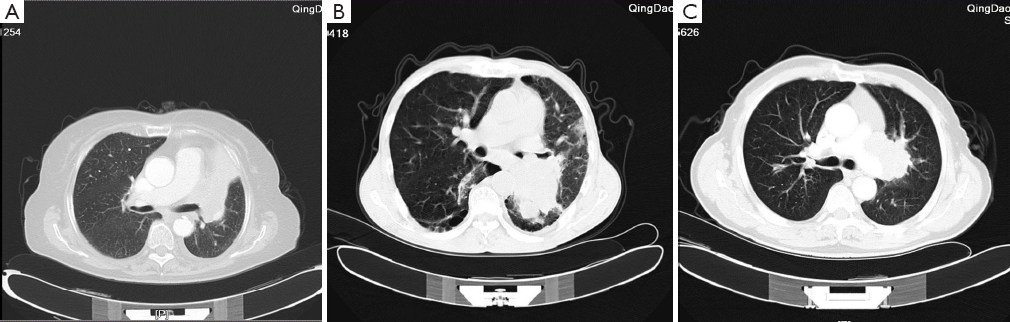
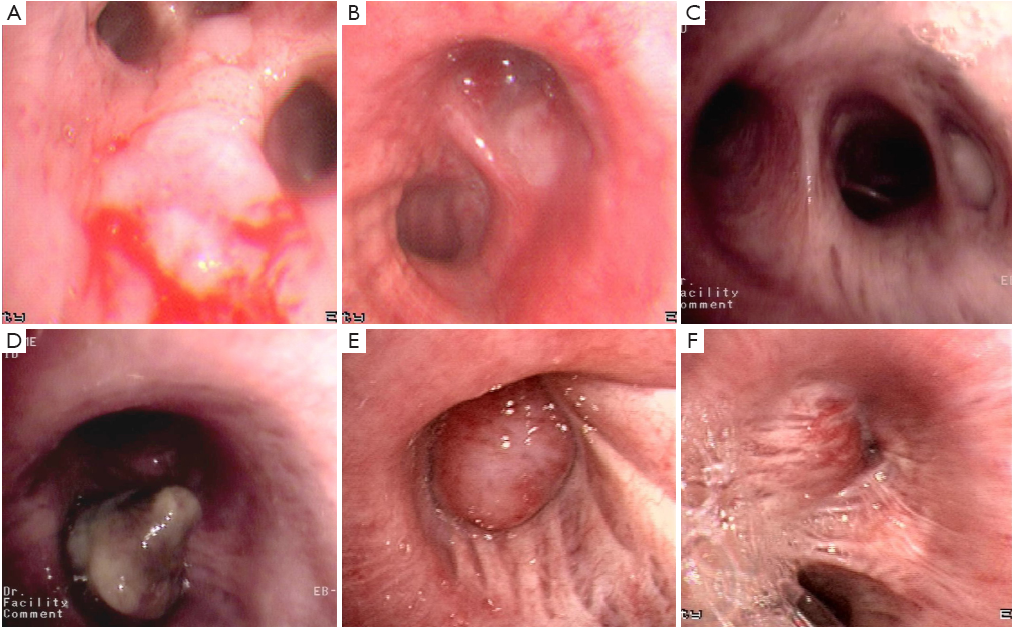
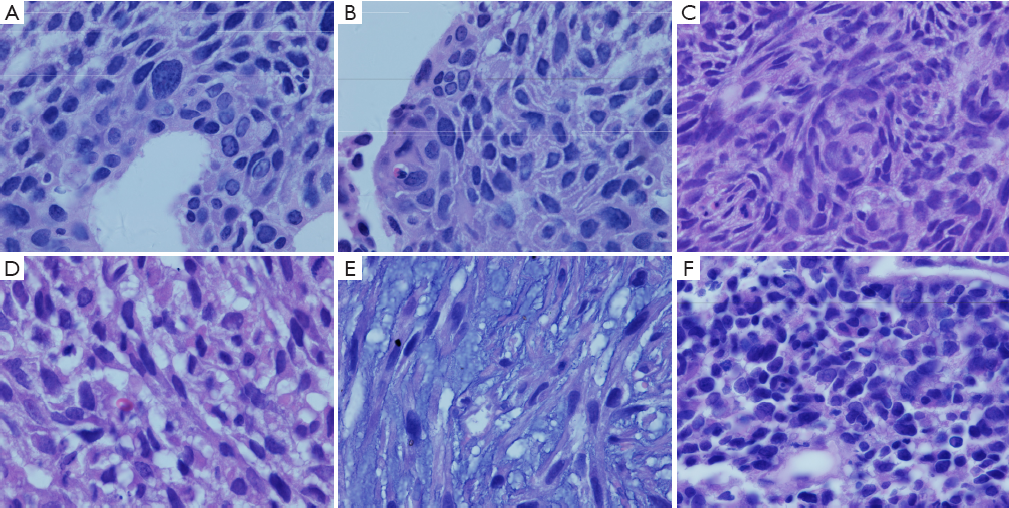
A 78-year-old woman with a history of smoking for 40 years (ten cigarettes daily) was admitted to our hospital because of persistent cough and fever. A CT scan of the chest revealed obstructive pneumonia and a small amount of pleural effusion in the left side (Figure 1A). However, no mediastinal lymph node enlargement was observed. Bronchoscopic examination showed a vesicle-like tumor at the bronchial orifice to the right upper lobe, with inter-segment, adherent growth and bleeding (Figure 2A). The left upper bronchus was completely obstructed by a polypoid mass (Figure 2B). All laboratory data were within the normal limits except for an elevated carcinoembryonic antigen level of 4.26 ng/mL. Biopsy specimens were collected from both lesions. Histological examination of the biopsy specimens revealed a well-differentiated squamous cell carcinoma (Figure 3A) in the right lung and a small cell lung carcinoma (Figure 3B) in the left lung. No metastatic lesions were noted on brain CT, cardiac and abdominal B-mode ultrasonography, or bone scanning.
Case 2
A 62-year-old man with a history of smoking for 42 years (30 cigarettes daily on average) was hospitalized because of persistent cough and hemoptysis for one week. CT revealed a polypoid mass in each of the lungs in addition to obstructive pneumonia and enlargement of multiple mediastinal lymph nodes (Figure 1B). Bronchoscopy showed a cauliflower-like mass with white furry coatings in the lower lobe of the right lung (Figure 2C) and a large mass obstructing the left main bronchus (Figure 2D). Laboratory studies indicated elevated levels of cytokeratin-19 fragment (CYFRA21-1, 7.87 ng/mL), cancer antigen (CA)-125 (63.56 U/mL), and CA199 (35.26 U/mL). Pathological findings confirmed a basaloid squamous cell carcinoma (Figure 3C) in the right lung and a carcinosarcoma (Figure 3D) in the left lung. Immunochemical staining of the left lung cancer showed positive reactions to epithelioid cell marker (P63 and cytokeratin) and fusiform cell marker (vimentin), as well as negative reactions to epithelial membrane antigen (EMA), desmin and S-100. The patient’s brain CT, heart and abdominal B-mode ultrasonography, and bone scanning showed no signs of distant metastasis.
Case 3
A 73-year-old man with a history of smoking of over 50 years (20 cigarettes per day on average) complained of persistent cough with sputum expectoration over the previous two months. CT revealed a mass in the left hilum, enlargement of multiple mediastinal lymph nodes, and a small amount of pleural effusion (Figure 1C). Bronchoscopic examination showed an endobronchial tumor with a smooth surface in the upper lobe of the right lung (Figure 2E), which completely blocked the airway branch, and another mass with a less smooth surface (Figure 2F) in the upper lobe of the left lung. Pathological study with immunohistochemical staining indicated a carcinosarcoma which was negative to cytokeratin and weak-positive to vimentin in the right lung (Figure 3E) and a small cell carcinoma which was positive to synaptophysin and neuron-specific enolase and negative to chromogranin A in the left (Figure 3F). Further investigations for distant metastasis were unremarkable.
Discussion
In the cases reported here, the diagnosis of DPLC was primarily based on the guidelines by the American College of Chest Physicians on lung cancer published in 2003 (3), which suggested such a diagnosis when (I) lesions of different histological types or molecular genetic characteristics found at the same time but originating from different carcinoma in situ or (II) lesions of the same histological type observed in different lobes, and neither N2-3 lymph node metastasis nor systemic metastasis detected. According to the chronological order of occurrence, DPLC can be classified as synchronous or metachronous (4). Each of the three DPLC patients reported here had carcinomas in different lobes with different histological types.
The incidence of DPLC has been reported to be approximately 0.2-20% in the western countries (5) and 0.3-1.2% in China (6,7). DPLC is often neglected or misdiagnosed as tumor metastasis or recurrence owing to the lack of knowledge and the limitation in diagnostic techniques and methods. According to current literature in China, surgical resection is the primary treatment option with the 5-year survival rate ranging from 14.3% to 66.4% (7-10). Lung CT is usually effective in identifying a single-mass lesion but can be less sensitive for small endotracheal lesions. Careful bronchial examination, particularly in long-term heavy smokers, is important. Tung et al. reported the importance of fiber-optic bronchoscopy, ultrasound-guided biopsy of the lesion for tissue examination, and positron emission tomography in diagnosing DPLC (11). All three patients reported herein presented with a long-term history of heavy smoking. CT revealed merely single occupying lesion in two of these patients, whereas the intra-tracheal lesion was discovered by fiber-optic bronchoscopy. If clinicians can identify the lesions and make accurate diagnoses earlier, proper care at an early stage may be delivered, and hence a better prognosis expected in the patients.
Patients with multiple lung tumours can present a diagnostic challenge for surgical pathologists. Discriminating between truely independent primary lung cancers and a primary tumour with satellite lesions or intrapulmonary metastases is of critical importance, as the clinical management and prognosis for these conditions varies significantly (12). The pathological diagnoses for the three patients were well-differentiated squamous cell carcinoma plus small cell lung cancer, squamous cell carcinoma plus carcinosarcoma, and carcinosarcoma plus small cell lung cancer, located in different lobes in each case. By tumor sites, squamous cell carcinoma was identified in the right upper (n=1) and lower (n=1) lobes, small cell lung cancer detected in the left upper lobe (n=2), and carcinosarcoma located in the right upper lobe (n=1) and in the left main bronchus (n=1), respectively. Our data further indicated that DPLC usually occurred in the upper lobes, with squamous cell carcinoma and small cell lung cancer being the more common histotypes. In addition, no reports on carcinosarcoma in DPLC were available, except for results on localized cancers (9,13). From the cases reported herein, we speculated that (I) male patients with a heavy smoking history (especially those with a ≥1,000 cigarette-years) were more likely to have carcinosarcoma; (II) carcinosarcomas were often larger in size and readily caused airway occlusion; and (III) patients diagnosed with carcinosarcoma might experience lymph node metastasis earlier, and their prognosis could be poorer than that of patients with other types of lung cancer; (IV) carcinosarcoma could be usually difficult to be distinguished from primary lung cancer, and therefore, immunohistochemical analysis should be needed.
Unfortunately, molecular biological studies were not available in our institution. Future studies should be warranted to analyze the gene mutations in DPLC, especially for those with carcinosarcoma, to shed light on the mechanisms underlying the pathogenesis of this condition, and to investigate the role of targeted therapy in these patients.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Simone CB 2nd, Friedberg JS, Glatstein E, et al. Photodynamic therapy for the treatment of non-small cell lung cancer. J Thorac Dis 2012;4:63-75. [PubMed]
- Usuda J, Ichinose S, Ishizumi T, et al. Management of multiple primary lung cancer in patients with centrally located early cancer lesions. J Thorac Oncol 2010;5:62-8. [PubMed]
- Detterbeck FC, Jones DR, Kernstine KH, et al. Lung cancer. Special treatment issues. Chest 2003;123:244S-258S. [PubMed]
- Huang J, Behrens C, Wistuba I, et al. Molecular analysis of synchronous and metachronous tumors of the lung: impact on management and prognosis. Ann Diagn Pathol 2001;5:321-9. [PubMed]
- Chang YL, Wu CT, Lee YC. Surgical treatment of synchronous multiple primary lung cancers: experience of 92 patients. J Thorac Cardiovasc Surg 2007;134:630-7. [PubMed]
- Zhang L, Li WT, Ding JA, et al. Surgical treatment of multiple primary lung cancer. Zhonghua Xiong Xin Waike Za Zhi 2004;20:59.
- Wang Y, Wang L, Zhang D. Diagnosis and surgical treatment of double primary lung cancer. Zhonghua Zhong Liu Za Zhi 2001;23:428-30. [PubMed]
- Feng FY, Zhang DC, Liu XY, et al. Surgical treatment and prognosis of synchronous double primary lung cancer: a report of 31 cases. Ai Zheng 2005;24:215-8. [PubMed]
- Wang SG, Wang CL. Clinical analysis about 32 double primary lung cancers. Zhonghua Zhong Liu Za Zhi 2008;35:259-61.
- Li F, Shao K, He J. The outcome of surgical therapy for double primary lung cancer. Zhonghua Wai Ke Za Zhi 2011;49:535-8. [PubMed]
- Tung YW, Hsu CP, Shai SE, et al. Surgical feasibility of ipsilateral multifocal non-small cell lung cancer in different lobes: excellent survival in node-negative subgroup. Eur J Cardiothorac Surg 2003;24:1008-12. [PubMed]
- Davidson MR, Gazdar AF, Clarke BE. The pivotal role of pathology in the management of lung cancer. J Thorac Dis 2013;5:S463-78. [PubMed]
- Braakhuis BJ, Tabor MP, Kummer JA, et al. A genetic explanation of Slaughter’s concept of field cancerization: evidence and clinical implications. Cancer Res 2003;63:1727-30. [PubMed]
