ALK gene expression status in pleural effusion predicts tumor responsiveness to crizotinib in Chinese patients with lung adenocarcinoma
Introduction
Driver gene abnormality tests are the premise of targeted therapy for advanced non-small cell lung cancer (NSCLC). Tumor histological (surgical or biopsy), cytological, and even blood samples can all be used to test for tumor biomarkers (1-6). Among these, cytologic samples are very important for pathological diagnosis and gene mutation testing in advanced NSCLC, and have been recommended as suitable for epidermal growth factor receptor (EGFR) and anaplastic lymphoma kinase (ALK) gene testing by the College of American Pathologists, the International Association for the Study of Lung Cancer, and the Association for Molecular Pathology, with cell blocks being preferred over smear preparations (7).
Pleural involvement with malignant pleural effusion (MPE) is a common manifestation of stage IV NSCLC. For many patients, MPE may be the only material available for diagnostic and molecular testing (8,9). Most MPE samples contain numerous tumor cells (high tumor content samples), which are not only sufficient for pathological diagnosis, but also ideal for driver gene status tests (10-12). As the prevalence of ALK gene rearrangement is also more common in stage IV NSCLC, MPE samples may be appropriate for ALK gene rearrangement testing (13,14).
Based on the PROFILE 1007 (response rate 74%) and PROFILE 1014 (response rate 65%) clinical trials, crizotinib is recommended as first-line therapy for patients with ALK-positive NSCLC in the National Comprehensive Cancer Network (NCCN) Clinical Practice Guideline for NSCLC (15-17). Routine methods for detecting the ALK gene status include fluorescence in situ hybridization (FISH), reverse transcription-polymerase chain reaction (RT-PCR), quantitative RT-PCR, next-generation sequencing (NGS), and immunohistochemistry (IHC) (18,19). In comparison with other techniques, staining of specimens with a mature IHC platform, the Ventana IHC ALK (D5F3) system, has been reported to detect ALK expression with high sensitivity and specificity, strong intensity, and high interpretation concordance between evaluators (20). Although the Ventana IHC ALK (D5F3) platform was approved by the US Food and Drug Administration (FDA) for ALK gene expression testing in NSCLC patients in June 2015, in the 2016 NCCN guideline (version 4) for NSCLC, FISH is now the recommended method. IHC is stated to be a rapid prescreening method only, with an ALK-positive IHC result requiring confirmation by FISH (17). Thus, more evidence on the testing of histological and cytological samples and therapeutic data are necessary to support the Ventana IHC ALK (D5F3) platform as a diagnostic tool for ALK gene expression and its recommendation in the NCCN guideline for NSCLC.
To determine the ALK gene expression status in MPE samples and the prediction of therapeutic efficacy of crizotinib in ALK expression-positive patients by using the Ventana IHC ALK (D5F3) system, a relatively large number of MPE samples (N=313) from Chinese patients with stage IV lung adenocarcinoma were collected and evaluated in this study. In 11 patients who were ALK expression-positive, tumor responsiveness data with crizotinib therapy were recorded.
Materials and methods
Patients and samples
A total of 313 pleural effusion samples were collected to diagnose adenocarcinoma consistent with an origin in the lung via a combination of IHC staining results and clinical information. All of the samples were obtained from patients from eight hospitals in Beijing between December 1, 2013 and June 30, 2015. Cell blocks were successfully prepared, and the tumor cell content in the cell blocks was sufficient to perform the subsequent gene abnormality tests. Data on the patients' smoking status were obtained and patients were classified as either "smokers" (those who had smoked >100 cigarettes per lifetime) or "never smokers" (those who had smoked <100 cigarettes per lifetime).
The experimental use of human specimens for this study was approved by the Peking University People's Hospital Medical Ethics Committee. Written informed consent was obtained from all the subjects.
Cytologic pathological diagnostic procedures
Pleural samples of 100−500 mL were anticoagulated with heparin, and cytological smears were prepared to determine whether there were no tumor cells or a low or high content of tumor cells before formalin-fixed paraffin-embedded (FFPE) cell blocks were prepared. The low and high tumor content MPE samples were centrifuged (1,500 r/min, 10 min), fixed in 4% neutral formalin for 6 h, and embedded in paraffin.
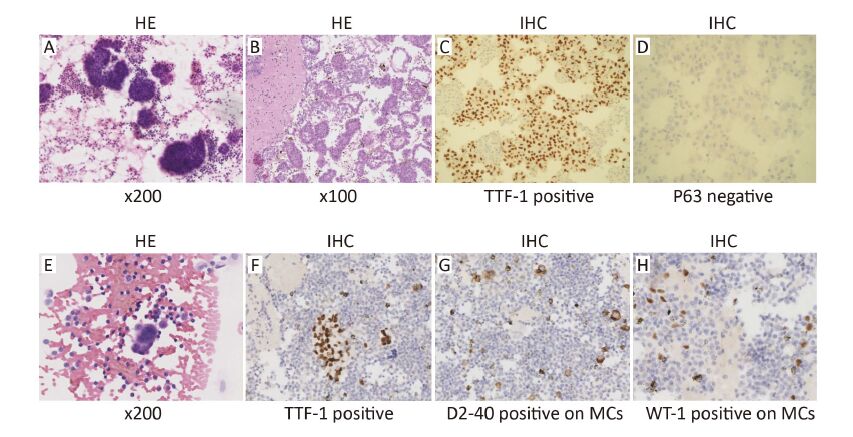
Tumor cells in the FFPE cell blocks were detected by hematoxylin and eosin (HE) staining, and the cytologic blocks were then divided into three groups: no tumor cells, low tumor content (tumor cells <20%), and high tumor content (tumor cells ≥20%). IHC staining was then applied to differentiate the origin and pathological typing of cell blocks with low and high tumor contents. Reactive mesothelial cells (MCs) and malignant pleural mesothelioma (MPM) were ruled out by routine IHC staining for cytokeratin 5 (CK5), Wilm's tumor-1 protein (WT-1) and podoplanin (D2−40) (biomarkers of mesothelial cell origin), and squamous cell carcinoma was ruled out by staining for P63 (a biomarker for squamous cell carcinoma). The biomarkers of lung adenocarcinoma tested for were CK7, thyroid transcription factor-1 (TTF-1), and napsin A. If the MPE was the first symptom that appeared, paired box 8 (PAX8) and caudal-type homeodomain transcription factor 2 (CDX2) for male patients and estrogen receptor (ER), progesterone receptor (PR), PAX8 and CDX2 for female patients were added to the antibody panel. For a pathological diagnosis of TTF-1-negative and napsin A-negative lung adenocarcinoma in MPE samples, MPM and adenocarcinomas from other organs were ruled out by IHC staining and by imaging data showing definite lung-occupying lesions.
Detection of ALK protein expression by IHC
FFPE cell blocks from the 313 MPE samples were stained by IHC with an anti-ALK monoclonal antibody (D5F3, Roche) and tested for ALK protein expression with the OptiView® DAB IHC Detection kit and the OptiView® Amplification kit (Ventana Medical Systems, Inc., Tucson, AZ, USA). In accordance with the manufacturer's instructions, FFPE sections (4 μm thick) were prepared for IHC staining, which was performed automatically using the Ventana BenchMark XT Stainer (Ventana Medical Systems Inc., Tucson, AZ, USA). The IHC stains were evaluated for ALK expression by two pathologists (DGL and ZW) who were trained to identify only strong cytoplasmic granular staining in tumor cells.
Detection of ALK rearrangement by FISH
All Ventana IHC ALK (D5F3)-positive MPE samples were also tested by FISH, which was carried out using the ALK Break Apart FISH Probe Kit (CytoTest Inc., USA). FFPE cell block sections (4 μm) were prepared for FISH staining according to the manufacturer's instructions. Positive cases were defined as those presenting split signals [5'-part (green fluorescence) and 3'-part (red fluorescence) signals were regarded as split when the separation distance was greater than 2 fluorescence signal diameters] or an isolated red signal in more than 15% of tumor cells. At least 50 tumor cells in each section were analyzed. Any atypical ALK FISH signal patterns were interpreted as negative signals. An "indefinite"ALK fusion status by FISH was judged when the cytologic samples were low tumor content (less than 20% in cytologic sections), tumor cells mingled with MCs and inflammatory cells, and differentiation of tumor cells from MCs and accurate calculation of the ratio of positive cells in the analyzed tumor cells were problematic in the dark fields of the fluorescence microscopy.
ARMS for EGFR mutation analysis
Screening for wild-type EGFR 18−21 exons in the 313 MPE samples was performed using the amplification refractory mutation system (ARMS). The ADx EGFR Mutations Detection Kit (Amoy Diagnostics, Xiamen, China) was employed to perform this analytical procedure. This kit covers 29EGFR mutation hotspots from exons 18 to 21, consisting of G719X (3 types), 19 deletions (19 types), 20 inserts (3 types), T790M, S768I, L858R and L861Q. Real-time direct sequencing PCR experiments were carried out using the ABI 7500 Fast PCR system (Applied Biosystems Inc., CA, USA). The Ct values used to determine whether a sample was positive or negative were based on extensive validation.
Statistical analysis
All statistical analyses were performed using SPSS Statistics software (Version 13.1; SPSS Inc., Chicago, IL, USA). Pearson's χ2 test and Fisher's exact test were performed to analyze variables. P<0.05 was considered statistically significant.
Results
Clinicopathological characteristics of the patients
The 313 pleural effusion samples were obtained from 163 females and 150 males aged 21 to 92 years (mean age, 64.19±13.14 years); 195 patients (62.3%) were ≥60 years old, and 118 (37.7%) were <60 years old. A smoking history was recorded in 132 patients (42.2%), while 181 (57.8%) had no smoking history. The pleural effusion samples were obtained following the first appearance of symptoms in 217 patients (69.3%), and in 196 cases (62.6%) they were only samples obtained for pathological diagnosis and gene status tests.
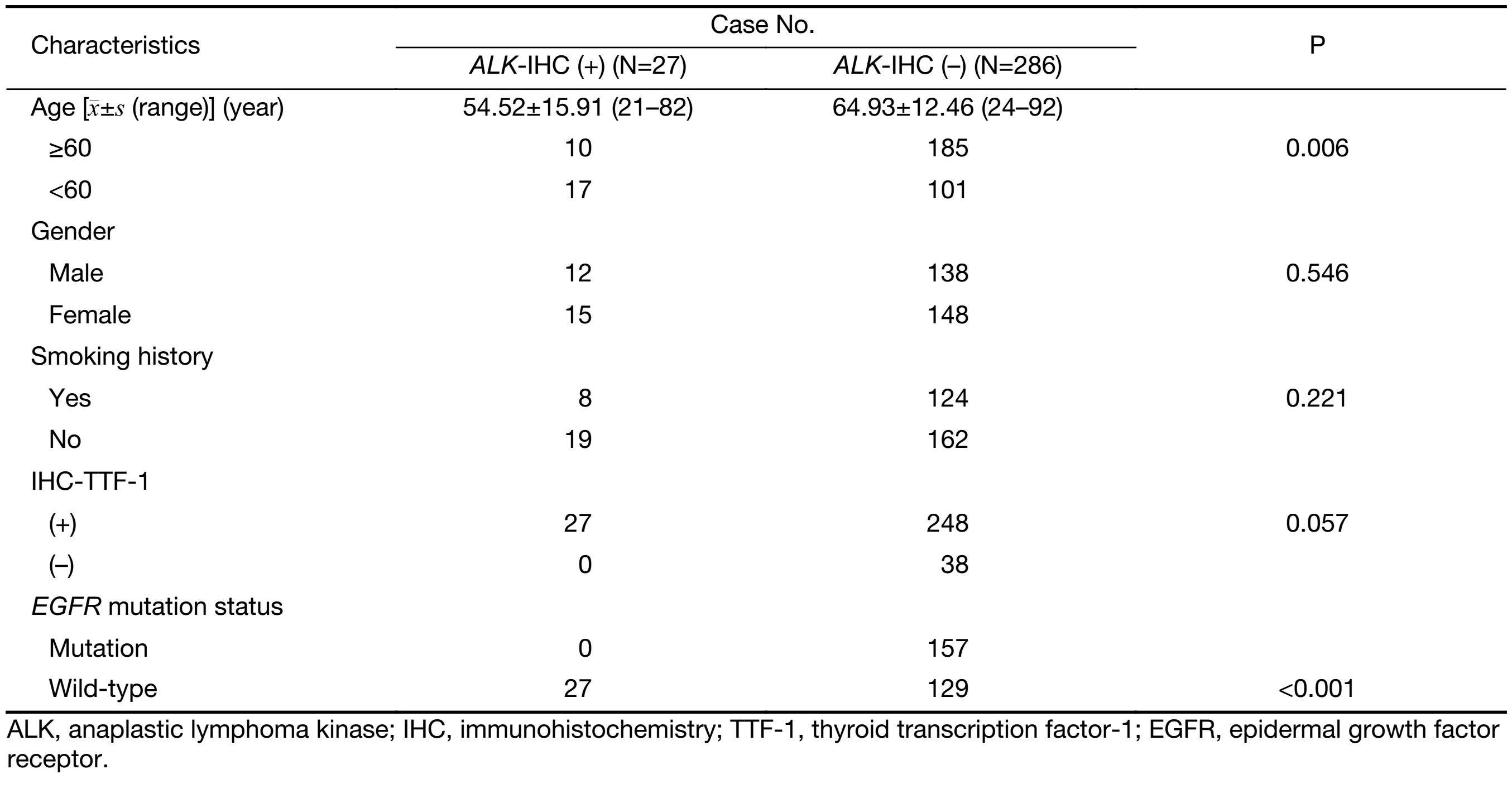
The clinicopathological characteristics of the patients according to whether they were Ventana IHC ALK (D5F3)-positive or-negative are summarized in Table 1.
Full table
Diagnosis of FFPE pleural effusion cytologic samples by IHC staining
All of the FFPE pleural effusion samples from the lung adenocarcinoma patients (100%) were CK7-positive, and 275 (87.9%) were identified as TTF-1 and/or napsin A expression-positive by IHC staining (Figure 1). Nine (2.9%) of the cytologic samples co-expressed P63 diffusely or focally. In 38 cases who were TTF-1- and napsin A-negative, imaging data revealed occupying lesions in the lung, and all 38 were CK5, WT-1, D2−40, P63, PAX8, and CDX2-negative and, in females, ER- and PR-negative as well. All 27 cytologic Ventana IHC ALK (D5F3)-positive samples showed positive expression of TTF-1, and 2 showed co-expression of P63.
ALK positive tests and clinicopathological characteristics
Ventana IHC (D5F3) analyses of ALK protein expression were successfully performed in all 313 of the FFPE pleural effusion cytologic samples. Ventana IHC ALK (D5F3)-positive results were identified by strong cytoplasmic granular staining in tumor cells, and 27 (8.6%) of the pleural effusion samples were ALK expression-positive. All of the positive signals were found to be strong and granular in the cytoplasm of adenocarcinoma cells, and they were homogeneous in staining intensity and extent (Figure 2). No heterogeneous tumor ALK expression was observed, even in low tumor content MPE samples. EGFR mutations were detected in 157 (50.2%) of the MPE samples. The Ventana IHC ALK (D5F3)-positive rate was 17.3% (27/156) in wild-type EGFR MPE samples. Simultaneous ALK expression and EGFR mutations were not detected in any of the 313 MPE samples.
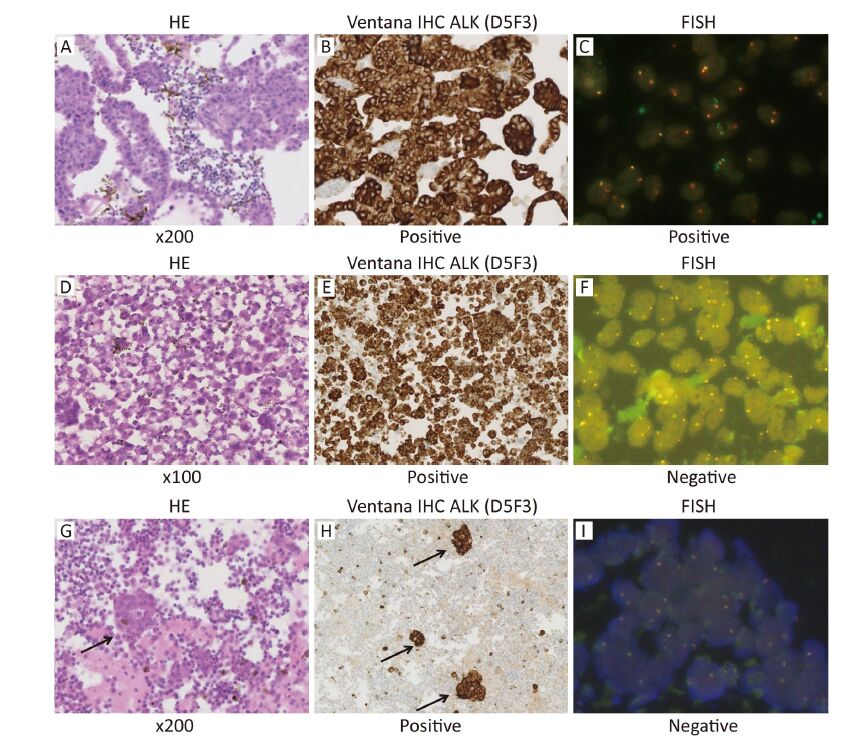
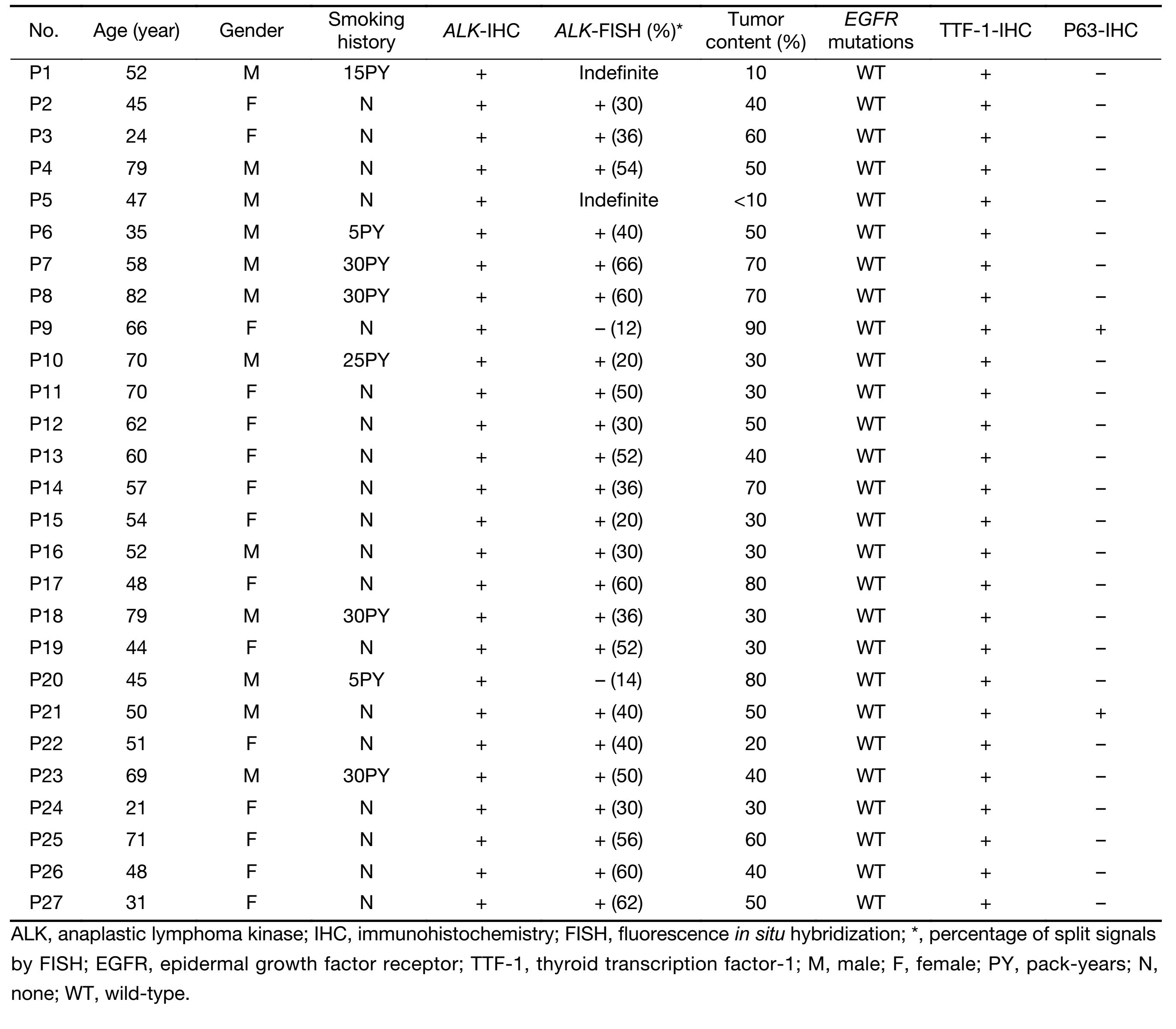
All 27 Ventana IHC ALK (D5F3)-positive MPE samples were tested by FISH (Figure 2). Of the 27 samples, 23 were interpreted as positive, and the percentages of ALK-positive nuclei in these 23 patients ranged from 20% to 66% (Table 2). Two patients (P9 and P20 in Table 2,3) were interpreted as FISH-negative. In these patients, next-generation sequencing was performed which confirmed the ALK fusion status, but the ALK rearrangement ratios were lower in these 2 patients. Results in the other 2 patients (P1 and P5 in Table 2,3) were interpreted as "indefinite". These 2 patients had low tumor content cell block sections, and it was difficult to differentiate tumor cells from MCs in the dark fields of the fluorescence microscope (Figure 2). The ALK rearrangement interpretations of the FISH test results by the two pathologists (ZW and DGL) showed concordance.
Full table
Full table
The clinicopathological characteristics of the 27 Ventana IHC ALK (D5F3)-positive patients are shown in Table 2. The mean age of these patients was 54.52 years old, whereas the mean age of the ALK (D5F3)-negative patients was 64.93 years old. The difference in the ALK-positive ratio between patients aged <60 years and ≥60 years was statistically significant (P=0.006; Fisher's exact test), as was the difference in the ALK-positive ratio between patients with wild-type EGFR and mutant-type EGFR (P<0.001; Fisher's exact test) (Table 1).
All 27 of the Ventana IHC ALK (D5F3)-positive patients were CK7- and TTF-1-positive, and 2 (7.4%) were also P63-positive. All 27 had wild-type EGFR gene.
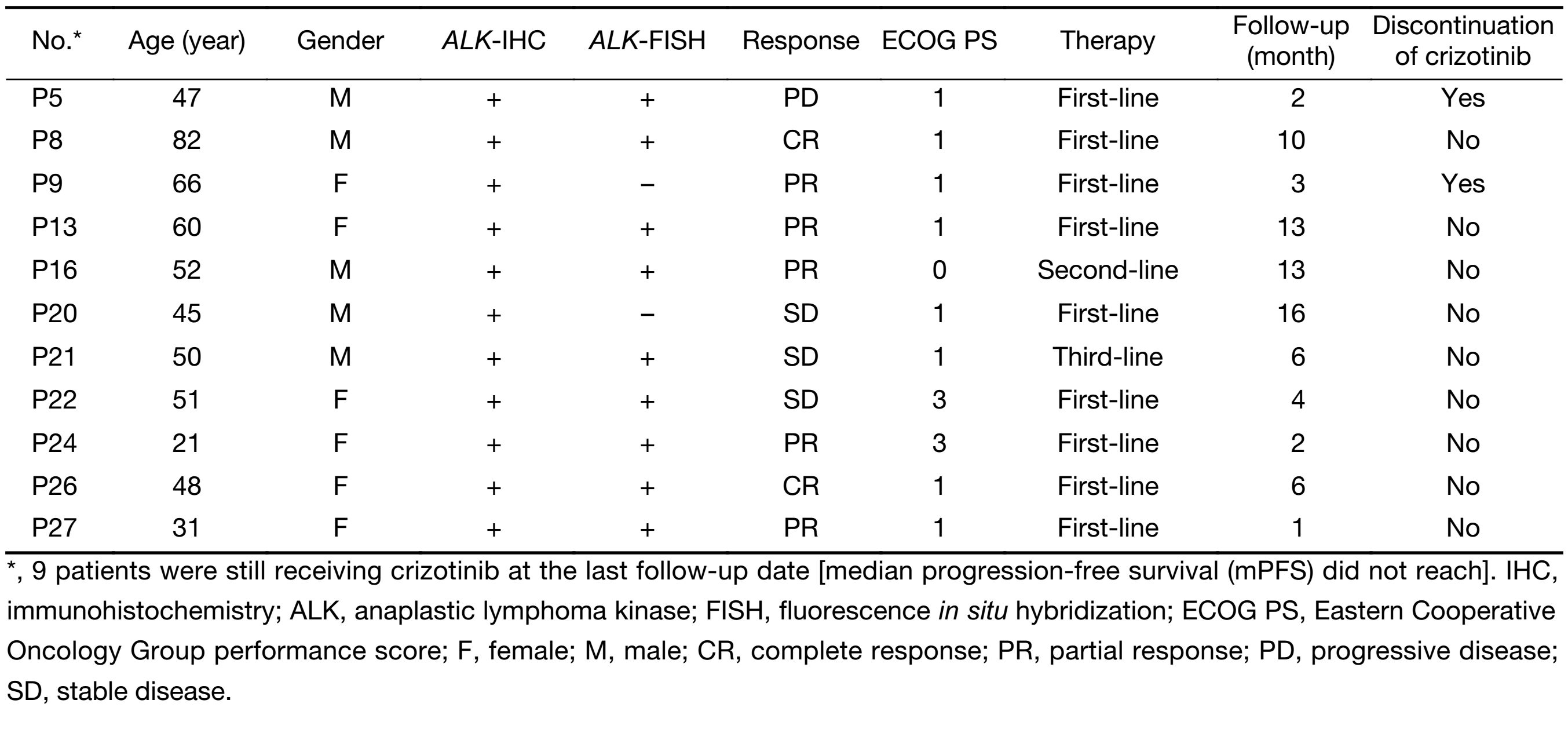
Responses to crizotinib treatment
Of the 27 Ventana IHC ALK (D5F3)-positive lung adenocarcinomas patients, 11 received crizotinib therapy. The responses to crizotinib are summarized in Table 3. The median Eastern Cooperative Oncology Group performance status (ECOG PS) score was 1 (range: 0−3) when crizotinib treatment was initiated; 9 patients received crizotinib as first-line treatment, while 2 patients had been treated previously (1 received critozinib as second-line therapy and 1 as third-line therapy). At the last follow-up date (June 30, 2015), 9 patients were still receiving crizotinib treatment. One patient (P9 in Table 2,3) died suddenly (due to pulmonary embolism or sudden cardiac death) after 3 months of treatment, and 1 (P5 in Table 2,3) discontinued treatment because of progressive disease after 2 months of treatment. The median follow-up time was 6.91 (range: 1−16) months. The median progression-free survival (mPFS) did not reach at the last follow-up date.
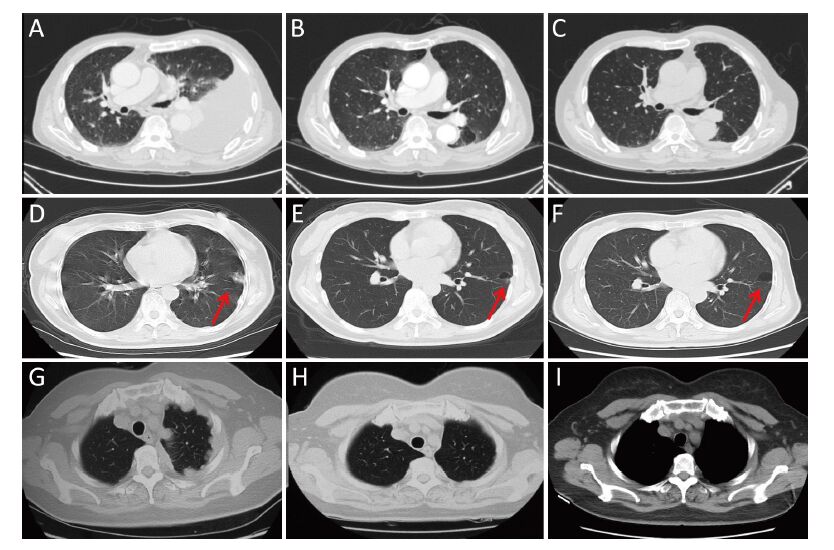
Among the 11 patients, 2 patients had complete response (CR) to crizotinib (follow-up time: 6 and 10 months, respectively), 5 had partial response (PR) (follow-up time: 1, 2, 3, 13 and 13 months, respectively), 3 had stable disease (SD) (follow-up time: 4, 6 and 16 months respectively), and 1 had progressive disease (PD) (follow-up time: 2 months) (Table 3). No grade 3 or 4 adverse events were observed with crizotinib therapy. The CT scanning results before and after crizotinib treatment in some patients are shown in Figure 3.
Discussion
Metastatic tumors from lung, breast, gastrointestinal and ovarian cancers, and MPM are the most common tumors of pleural membranes and the major causes of MPE (21,22). The diagnosis of lung adenocarcinoma in MPE has been discussed in the literature (23,24). MPE samples are now commonly used for diagnosis and molecular testing of NSCLC patients at stage IV. They have proved to be an ideal sample type for EGFR mutation testing in NSCLC (25,26). However, ALK rearrangements are relatively low-frequency mutations in NSCLC, and MPE samples for ALK gene status testing are not as well studied. Most published studies have focused on comparisons among the different assays. But this study investigated ALK expression in a relatively large number of MPE samples from patients with lung adenocarcinomas who were tested by the Ventana IHC ALK (D5F3) platform, and subsequent evaluation of the responsiveness to crizotinib (in 11 cases). The key findings of the study are: 1) the positive ALK expression rate was higher in MPE samples from patients with stage IV disease than from those with early stage lung adenocarcinoma; and 2) the use of only the Ventana IHC ALK (D5F3) platform to detect ALK expression may be sufficient to predict responsiveness to crizotinib, and thus other methods to verify the ALK status may not be necessary.
The positive ALK protein expression rate with the Ventana IHC ALK (D5F3) test platform was 8.6% (27/313) in the MPE samples tested in this study, and 17.3% (27/156) in the wild-type EGFR MPE samples. In some studies, EGFR mutations have been reported to be more common in pleural metastases and MPE samples than in primary tumors (27,28), while in other studies, KRAS mutations in MPE have been found to be lower than in primary tumors (29). Data from a meta-analysis have shown a statistically significant increase in the frequency of EML4-ALK mutations in stage III-IV NSCLC in comparison with stage I-II disease (8.2% vs. 4.0%) (30). The positive ALK protein expression rate in MPE samples using the Ventana IHC ALK (D5F3) platform in our study is consistent with this meta-analysis. Moreover, there were no instances of ALK expression being detected simultaneously with EGFR mutations in the 313 MPE samples tested.
Although there have been some previous case reports of the efficacy of ALK-tyrosine kinase inhibitor (TKI) therapy in patients in whom ALK protein expression was detected in MPE samples (31,32), we obtained efficacy data with crizotinib in a total of 11 lung adenocarcinoma patients who were Ventana IHC ALK (D5F3)-positive. Two patients had CR (2/11, 18.2%), 5 had PR (5/11, 45.5%), and 3 had SD (3/11, 27.3%). This result had approached the therapeutic efficacy of crizotinib for ALK-positive NSCLC reported in the PROFILE 1007 and 1014 studies. This suggests that crizotinib is effective in patients with advanced lung adenocarcinoma who are Ventana IHC ALK (D5F3)-positive in MPE samples. Our findings in a relatively large case series study of Chinese patients with advanced lung adenocarcinoma provide direct evidence of the relevance of ALK protein expression in MPE samples for predicting responsiveness to ALK-TKI therapy.
The Ventana IHC ALK (D5F3) test platform is both convenient and feasible for testing MPE samples, and shows high sensitivity (33,34). In this study, a comparison with FISH test results revealed that 4 patients were Ventana IHC ALK (D5F3)-positive but FISH-negative or "indefinite". The two FISH-indefinite results were in low-tumor content samples. We have discussed the possible reasons why low-tumor content MPE samples are not suitable for detecting ALK fusion by FISH in one of our previously published articles (35), and why the two ALK IHC-positive/FISH-negative patients obtained a therapeutic response with crizotinib in another article (36).
Although cell-transferred cytologic smears of lung adenocarcinoma were used for detecting ALK expression in a previous study (37), we recommend that FFPE cell blocks of MPE should be prepared, if possible, and the Ventana IHC ALK (D5F3) test platform should be used to test the ALK gene status in MPE samples. Ventana IHC ALK (D5F3) staining can show strong positive signals for interpreting the ALK gene status in even very low tumor content cell blocks of MPE samples (<10%). Interpretation of FISH tests results may also be a challenge with low tumor content MPE samples, as identification of cancer cells from MCs can be problematic in dark fields during fluorescence microscopy of MPE cell blocks.
Conclusions
In this study, the ALK gene status was tested in a relatively large number of MPE samples from Chinese patients with advanced lung adenocarcinoma, and the responsiveness to crizotinib was assessed in 11 Ventana IHC ALK (D5F3)-positive patients. The findings of the study could provide evidence of the relevance of Ventana IHC ALK (D5F3) testing of MPE samples for predicting the efficacy of ALK-TKI therapy. The responses achieved with crizotinib in the 11 patients suggest that this agent can be effectively used in advanced lung adenocarcinoma patients whose MPE samples are Ventana IHC ALK (D5F3)-positive.
Acknowledgements
We would like to thank Li Zhang, Zaiwen Fan, Lingyun Ma, Li Yang and Jing Di for their contributions to this study.
Funding: This study was supported by grants from the Beijing Municipal Science and Technology Commission (D141100000214003), and the Natural Science Foundation of China (No. 81641114).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Soda M, Choi YL, Enomoto M, et al. Identification of the transforming EML4-ALK fusion gene in non-small-cell lung cancer. Nature 2007;448:561–6. [PubMed] DOI:10.1038/nature05945
- Alì G, Proietti A, Pelliccioni S, et al. ALK rearrangement in a large series of consecutive non-small cell lung cancers: comparison between a new immunohistochemical approach and fluorescence in situ hybridization for the screening of patients eligible for crizotinib treatment. Arch Pathol Lab Med 2014;138:1449–58. [PubMed] DOI:10.5858/arpa.2013-0388-OA
- Malapelle U, Bellevicine C, De Luca C, et al. EGFR mutations detected on cytology samples by a centralized laboratory reliably predict response to gefitinib in non-small cell lung carcinoma patients. Cancer Cytopathol 2013;121:552–60. [PubMed] DOI:10.1002/cncy.21322
- Tseng JS, Yang TY, Tsai CR, et al. Dynamic plasma EGFR mutation status as a predictor of EGFR-TKI efficacy in patients with EGFR-mutant lung adenocarcinoma. J Thorac Oncol 2015;10:603–10. [PubMed] DOI:10.1097/JTO.cjcr-28-6-60600443
- Karachaliou N, Mayo-de las Casas C, Queralt C, et al. Association of EGFR L858R mutation in circulating free DNA with survival in the EURTAC trial. JAMA Oncol 2015;1:149–57. [PubMed] DOI:10.1001/jamaoncol.2014.257
- Thress KS, Paweletz CP, Felip E, et al. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non-small cell lung cancer harboring EGFR T790M. Nat Med 2015;21:560–2. [PubMed] DOI:10.1038/nm.3854
- Lindeman NI, Cagle PT, Beasley MB, et al. Molecular testing guideline for selection of lung cancer patients for EGFR and ALK tyrosine kinase inhibitors: guideline from the College of American Pathologists, International Association for the Study of Lung Cancer, and Association for Molecular Pathology. J Thorac Oncol 2013;8:823–59. [PubMed] DOI:10.1097/JTO.0b013e318290868f
- Chen YL, Lee CT, Lu CC, et al. Epidermal growth factor receptor mutation and anaplastic lymphoma kinase gene fusion: detection in malignant pleural effusion by RNA or PNA analysis. PLoS One 2016;11:e0158125. [PubMed] DOI:10.1371/journal.pone.0158125
- Zarogoulidis K, Zarogoulidis P, Darwiche K, et al. Malignant pleural effusion and algorithm management. J Thorac Dis 2013;5:S413–9. [PubMed] DOI:10.3978/j.issn.2072-1439.2013.09.04
- Akamatsu H, Koh Y, Kenmotsu H, et al. Multiplexed molecular profiling of lung cancer using pleural effusion. J Thorac Oncol 2014;9:1048–52. [PubMed] DOI:10.1097/JTO.cjcr-28-6-60600203
- Agalioti T, Giannou AD, Stathopoulos GT. Pleural involvement in lung cancer. J Thorac Dis 2015;7:1021–30. [PubMed] DOI:10.3978/j.issn.2072-1439.2015.04.23
- Tsai TH, Wu SG, Hsieh MS, et al. Clinical and prognostic implications of RET rearrangements in metastatic lung adenocarcinoma patients with malignant pleural effusion. Lung Cancer 2015;88:208–14. [PubMed] DOI:10.1016/j.lungcan.2015.02.018
- Fan L, Feng Y, Wan H, et al. Clinicopathological and demographical characteristics of non-small cell lung cancer patients with ALK rearrangements: a systematic review and meta-analysis. PLoS One 2014;9:e100866. [PubMed] DOI:10.1371/journal.pone.0100866
- Zhou J, Yao H, Zhao J, et al. Cell block samples from malignant pleural effusion might be valid alternative samples for anaplastic lymphoma kinase detection in patients with advanced non-small-cell lung cancer. Histopathology 2015;66:949–54. [PubMed] DOI:10.1111/his.2015.66.issue-7
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167–77. [PubMed] DOI:10.1056/NEJMoa1408440
- Frampton JE. Crizotinib: a review of its use in the treatment of anaplastic lymphoma kinase-positive, advanced non-small cell lung cancer. Drugs 2013;73:2031–51. [PubMed] DOI:10.1007/s40265-013-0142-z
- National Comprehensive Cancer Network. NCCN Guidelines. Non-small cell lung cancer, version 4, 2016. Available at: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf
- Le Quesne J, Maurya M, Yancheva SG, et al. A comparison of immunohistochemical assays and FISH in detecting the ALK translocation in diagnostic histological and cytological lung tumor material. J Thorac Oncol 2014;9:769–74. [PubMed] DOI:10.1097/JTO.cjcr-28-6-60600157
- Tuononen K, Sarhadi VK, Wirtanen A, et al. Targeted resequencing reveals ALK fusions in non-small cell lung carcinomas detected by FISH, immunohistochemistry, and real-time RT-PCR: a comparison of four methods. Biomed Res Int 2013;2013:757490. [PubMed] DOI:10.1155/2013/757490
- Wynes MW, Sholl LM, Dietel M, et al. An international interpretation study using the ALK IHC antibody D5F3 and a sensitive detection kit demonstrates high concordance between ALK IHC and ALK FISH and between evaluators. J Thorac Oncol 2014;9:631–8. [PubMed] DOI:10.1097/JTO.cjcr-28-6-60600115
- Assis LV, Isoldi MC. Overview of the biochemical and genetic processes in malignant mesothelioma. J Bras Pneumol 2014;40:429–42. [PubMed] DOI:10.1590/S1806-37132014000400012
- Roberts ME, Neville E, Berrisford RG, et al. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii32–40. [PubMed] DOI:10.1136/thx.2010.136994
- Karpathiou G, Stefanou D, Froudarakis ME. Pleural neoplastic pathology. Respir Med 2015;109:931–43. [PubMed] DOI:10.1016/j.rmed.2015.05.014
- Porcel JM, Palma R, Bielsa S, et al. TTF-1 and napsin A on cell blocks and supernatants of pleural fluids for labeling malignant effusions. Respirology 2015;20:831–3. [PubMed] DOI:10.1111/resp.2015.20.issue-5
- Wu SG, Yu CJ, Tsai MF, et al. Survival of lung adenocarcinoma patients with malignant pleural effusion. Eur Respir J 2013;41:1409–18. [PubMed] DOI:10.1183/09031936.00069812
- Jian G, Songwen Z, Ling Z, et al. Prediction of epidermal growth factor receptor mutations in the plasma/pleural effusion to efficacy of gefitinib treatment in advanced non-small cell lung cancer. J Cancer Res Clin Oncol 2010;136:1341–7. [PubMed] DOI:10.1007/s00432-010-0785-z
- Zou J, Bella AE, Chen Z, et al. Frequency of EGFR mutations in lung adenocarcinoma with malignant pleural effusion: Implication of cancer biological behaviour regulated by EGFR mutation. J Int Med Res 2014;42:1110–7. [PubMed] DOI:10.1177/0300060514539273
- Han HS, Eom DW, Kim JH, et al. EGFR mutation status in primary lung adenocarcinomas and corresponding metastatic lesions: discordance in pleural metastasis. Clin Lung Cancer 2011;12:380–6. [PubMed] DOI:10.1016/j.cllc.2011.02.006
- Lozano MD, Zulueta JJ, Echeveste JI, et al. Assessment of epidermal growth factor receptor and K-ras mutation status in cytological stained smears of non-small cell lung cancer patients: correlation with clinical outcomes. Oncologist 2011;16:877–85. [PubMed] DOI:10.1634/theoncologist.2010-0155
- Zhao F, Xu M, Lei H, et al. Clinicopathological characteristics of patients with non-small-cell lung cancer who harbor EML4-ALK fusion gene: a meta-analysis. PLoS One 2015;10:e0117333. [PubMed] DOI:10.1371/journal.pone.0117333
- Wang W, Tang Y, Li J, et al. Detection of ALK rearrangements in malignant pleural effusion cell blocks from patients with advanced non-small cell lung cancer: a comparison of Ventana immuno-histochemistry and fluorescence in situ hybridization. Cancer Cytopathol 2015;123:117–22. [PubMed] DOI:10.1002/cncy.21510
- Takakuwa O, Oguri T, Yokoyama M, et al. Esophagitis resulting from treatment with crizotinib for anaplastic lymphoma kinase rearrangement-positive lung adenocarcinoma: A case report. Mol Clin Oncol 2014;2:121–3. [PubMed] DOI:10.3892/mco.2013.188
- Ying J, Guo L, Qiu T, et al. Diagnostic value of a novel fully automated immunochemistry assay for detection of ALK rearrangement in primary lung adenocarcinoma. Ann Oncol 2013;24:2589–93. [PubMed] DOI:10.1093/annonc/mdt295
- von Laffert M, Warth A, Penzel R, et al. Multicenter immunohistochemical ALK-testing of non-small-cell lung cancer shows high concordance after harmonization of techniques and interpretation criteria. J Thorac Oncol 2014;9:1685–92. [PubMed] DOI:10.1097/JTO.cjcr-28-6-60600332
- Wang Z, Wu X, Shi Y, et al. Ventana immuno-histochemistry ALK (D5F3) detection of ALK expression in pleural effusion samples of lung adenocarcinoma. Per Med 2015;12:349–57. DOI:10.2217/pme.15.3
- Ma D, Wang Z, Yang L, et al. Responses to crizotinib in patients with ALK-positive lung adenocarcinoma who tested immunohistochemistry (IHC)-positive and fluorescence in situ hybridization (FISH)-negative. Oncotarget 2016. [Epub ahead of print].
- Zhang C, Randolph ML, Jones KJ, et al. Anaplastic lymphoma kinase immunocytochemistry on cell-transferred cytologic smears of lung adenocarcinoma. Acta Cytol 2015;59:213–8. [PubMed] DOI:10.1159/000430083
