Clinical value of contrast-enhanced ultrasound in improving diagnostic accuracy rate of transthoracic biopsy of anterior-medial mediastinal lesions
Introduction
The mediastinum is the central portion of the thoracic cavity, limited by pleural cavities laterally, thoracic inlet superiorly, and the diaphragm inferiorly. Mediastinal lesions are a common type of diseases in thoracic surgery. Correct pathological diagnosis is of vital importance for determining the proper therapeutic option. In recent years, ultrasound-guided transthoracic biopsy of mediastinal lesions has attracted clinical attention due to its advantages of being economic, convenient, safe, quick, and no radiation (1-3). However, conventional ultrasound (US) cannot clearly reveal the internal structures of the mediastinal lesions and the detection of superficial vessels or presence of internal necrotic tissue was limited (4). As a consequence, there is a risk of complications, such as bleeding, or false-negative results of biopsy.
Contrast-enhanced ultrasound (CEUS) is now employed widely for the diagnosis of solid tumors. After intravenous injection of contrast agent, SonoVue, ultrasound can provide very useful information for both macrovasculature and microvasculature. CEUS could continuously monitor the dynamic perfusion of the lesions in real time and increase diagnostic accuracy than conventional ultrasound (5-7). Several investigators reported that CEUS also improved the diagnostic accuracy of the biopsy procedure in the liver or other organs (5,8-11), because it can help differentiate viable from necrotic tissues. In this study, we evaluate the clinical value of CEUS in transthoracic biopsy of mediastinal lesions. Lesions in posterior mediastinum are vulnerable to be blocked by the lung and bone. Therefore the lesions in posterior mediastinum are difficult to be shown by ultrasound. The patients who were recommended for ultrasound-guided transthoracic biopsy mainly have anterior and medial mediastinal lesions. We examined 123 patients with anterior-medial mediastinal lesions who intend to receive biopsy for pathological diagnosis, analyzed the perfusion features of the CEUS group and explored the clinical value of CEUS in improving biopsy diagnostic accuracy of anterior-medial mediastinal lesions.
Materials and methods
Patients
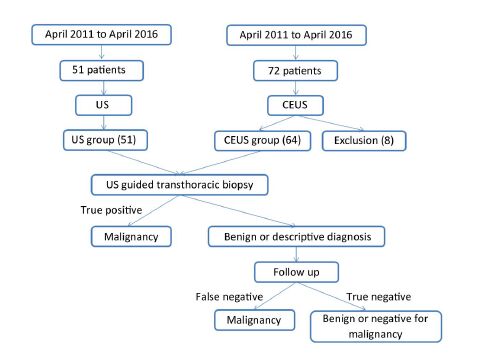
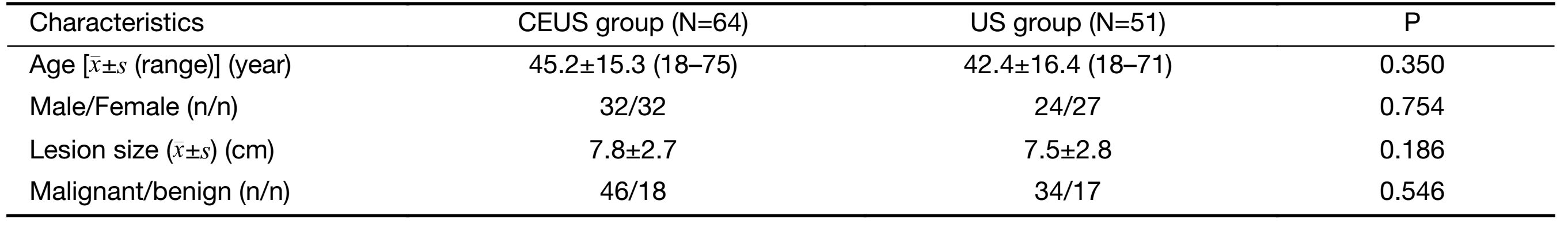
From April 2011 to April 2016, 123 patients who were diagnosed with anterior-medial mediastinal lesions by chest computed tomography (CT) and were recommended for ultrasound-guided transthoracic biopsy in the Department of Ultrasound, Peking University Cancer Hospital were enrolled in this study. Among them, 72 patients underwent CEUS before biopsy, of whom 8 cases were found not suitable for needle biopsy. As a consequence, the rest 64 cases were recruited into the CEUS group, including 32 males and 32 females, aged 18−75 years old (mean: 45.2±15.3 years), with a mean lesion size of 7.8±2.7 cm. At the same period, the other 51 patients who received conventional ultrasound-guided biopsy without CEUS were regarded as the US group. These patients refused CEUS because of economic factors after fully explaining the advantages and risks of CEUS application. There were 24 males and 27 females, aged 18−71 years old (mean: 42.4±16.4 years), with a mean lesion size of 7.5±2.8 cm. Figure 1 summarizes the patients selected in this study. There was no statistically significant difference in clinical characteristics between the CEUS group and the US group (Table 1).
Full table
This study was approved by the Research and Ethics Committee of Peking University Cancer Hospital, and written informed consent was obtained from each patient before the CEUS examination and biopsy procedures.
Contrast agent and sonography procedures
For the CEUS group, patients underwent CEUS examination 30−60 min before the biopsy. SonoVue (Bracco SpA, Milan, Italy) was used as the sonography contrast agent, supplied as a lyophilized powder and reconstituted with 5 mL of saline to form a homogeneous microbubble suspension that contains 8 μL/mL sulfur hexafluoride stabilized by a phospholipid shell. SonoVue was administered intravenously as 1.5 mL boluses through the antecubital vein in 2−3 s. Logiq E9 sonography system (GE, USA) with real-time gray-scale contrast tuned imaging and a 3.0−5.0 MHz C5−1 probe (GE, USA) were used when CEUS was performed.
Chest CT was performed in all patients before our study. With the reference of chest CT, conventional sonography was performed to investigate the location, texture and size of the lesion. Contrast-enhanced imaging was then initiated, and the acoustic power output was adjusted to about 0.11 to 0.13 mechanical indexes on the basis of the lesion depth and body habitus of the patient. After contrast agent administration, the perfusion and enhancement patterns, necrosis (anechoic) area of the target lesions and nearby structures were observed about 5 min in real time. The conventional ultrasound images were recorded by still images and dynamic images. The CEUS images were recorded by dynamic images with digital imaging and communications in medicine (DICOM) format. CEUS analysis was performed on the basis of review of stored sonographic clips. Patterns of enhancement were evaluated by 2 observers (W.Y. and S.W.), who reached a consensus with emphasis on the presence of necrotic (anechoic) areas.
In both groups, the biopsy puncture plan was established by collecting the information of the location and size of lesions, necrosis area, pericardial effusion and superficial vessels.
Biopsy indication and method
The indications for ultrasound-guided transthoracic biopsy of anterior-medial mediastinal lesions were as follows: 1) accessibility of lesions via a transthoracic approach with ultrasound; 2) a lesion larger than 2 cm in diameter; 3) a lesion with mixture texture has at least 2 cm thickness of solid content; 4) a patient can well control breath; 5) no superficial large vessel in the puncture path; and 6) platelet count was greater than 60×109/L.
In the US group, conventional ultrasound (including color Doppler imaging) was routinely used for selection of an optimal biopsy path. The sampling site was localized according to the sonographic appearance (solid part of the lesion with the shortest pathway). In the CEUS group, besides conventional ultrasound, the information from contrast-enhanced sonography was also used to select the biopsy path and sampling site (solid part of the lesion with the shortest pathway).
For the biopsy procedures in this study, sonography system Logiq E9 (GE, USA) with 3.5−5.0 MHz small-sector convex probes accessorized with biopsy was used to provide sonographic guidance. Biopsy was performed using an 18-gauge automatic cutting needle (Bard Magnum, Bard, USA). After careful planning, the skin was sterilized, and local anesthesia was applied using 5 mL of 1% lidocaine (Liduokayin; Yimin Pharmaceutical Co., Ltd, Beijing, China). After the probe was fixed and the guiding needle was inserted into the chest wall, the biopsy needle was inserted for biopsy. It should be noted that the biopsy route should avoid damaging large blood vessels and advance into the target area under real-time visualization. The number of puncture attempts was decided by the quantity and color of the specimen obtained. The puncture attempts were no more than 3 times. The specimens obtained during the biopsy were fixed in 10% formalin.
The patient stayed in the hospital for at least 1 h to monitor whether there was complication after biopsy. The specimens were sent to the Department of Pathology for histologic examinations by two experienced pathologists. The second or third session of biopsy required if the initial biopsy could not get definite diagnosis.
Imaging evaluation
The conventional ultrasound and CEUS features were summarized and compared. It was defined as necrosis in CEUS group if CEUS showed the lesion was complete absence of enhancement during arterial phase and parenchymal phase (12). It was defined as necrosis in US group if conventional ultrasound showed there was anechoic area within lesions, clear boundaries, and color Doppler flow imaging (CDFI) showed no blood flow within the anechoic area. Contrast-enhanced CT was adopted as the diagnosis criterion for the detection rate of necrosis in lesions.
Final diagnosis
The final diagnosis was made as definite diagnosis, descriptive diagnosis, and unable diagnosis based on comprehensive diagnosis of all pathological specimens from two experienced pathologists. Definite diagnosis was considered correct if the pathologic diagnosis confirmed malignancy. Benign diagnosis and descriptive diagnosis need to be confirmed with other imaging examinations and 6 months of follow-up. If the other imaging examination and follow-up confirm the diagnosis, the diagnosis was considered correct. If no tissues or undeterminable necrotic tissues were described in the descriptive diagnosis, the diagnosis was considered failure.
Statistical analysis
All analyses were performed using IBM SPSS Statistics (Version 21.0; IBM Corp., New York, USA). Numerical data were given as x±s and were analyzed with independent samples t-test or paired t-test. Categorical variables were analyzed with Pearson χ2 and Fisher's exact test. P<0.05 was considered statistically significant.
Results
Biopsy indication selection with CEUS
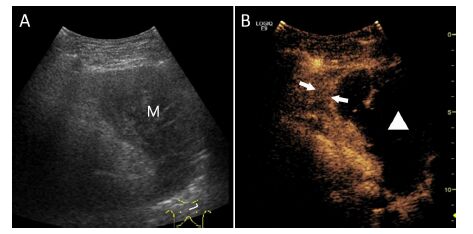
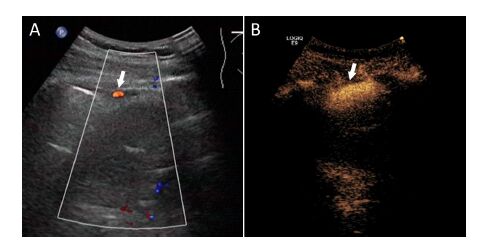
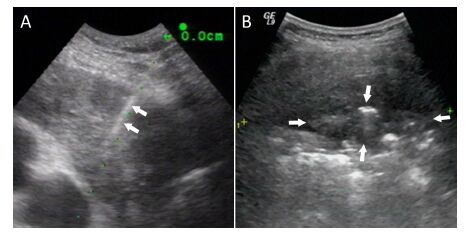
After the CEUS examination, 8 of the 72 patients were excluded from ultrasound-guided transthoracic biopsy. Of them, 5 patients had the lesions with more than 80% of the necrotic portion (Figure 2), and another 3 patients had superficial large vessels at puncture path which were difficult to avoid (Figure 3). The remaining 64 patients underwent biopsy within 30−60 min.
Features of ultrasound images
The tumor sizes of the CEUS group and the US group were 7.8±2.7 cm and 7.5±2.8 cm, respectively (P=0.186). The detection rate of internal necrosis in the CEUS group (43.8%, 28/64) was statistically higher than that of the US group (11.8%, 6/51) (P<0.001). Based on the sizes of the lesions, the cases were further subdivided. For lesions ≤5 cm in diameter, the necrosis rate was only 14.3% (1/7) in CEUS group and 11.1% (1/9) in US group (P=1.000). For lesions >5 cm in diameter, the detection rate of necrosis in CEUS group (47.4%, 27/57) was significantly higher than that of US group (11.9%, 5/42) (P<0.001). With the lesion size increased, the detection rate of necrosis in lesions increased by CEUS (Table 2).
Full table
Based on the finial diagnosis, there were 46 cases had malignant lesions and 18 cases had benign lesions in the CEUS group, and 34 cases had malignant lesions and 17 cases had benign lesions in US group (Table 3).
Full table
Next we summarized the CEUS features of different histopathology lesions, including lymphoma, thymoma and thymic carcinoma, which are commonly found in anterior-medial mediastinum. Compared with lymphoma and thymic carcinoma, a majority of thymoma cases had homogenous enhancement patterns in the arterial phase (100% vs. 56.5%, P=0.006; 100% vs. 25.0%, P<0.001). Compared with thymic carcinoma, thymoma had less frequency to be found having the internal necrosis (7.1% vs. 75.0%, P<0.001) (Table 4). In addition, compared with conventional ultrasound, CEUS increased the detection rate for internal necrosis (62.5% vs. 18.8%, P=0.029) and pericardial effusion (56.3% vs. 12.5%, P=0.023) in thymic carcinoma (Table 5).
Full table
Full table
Number of biopsy puncture attempts and diagnostic accuracy rate
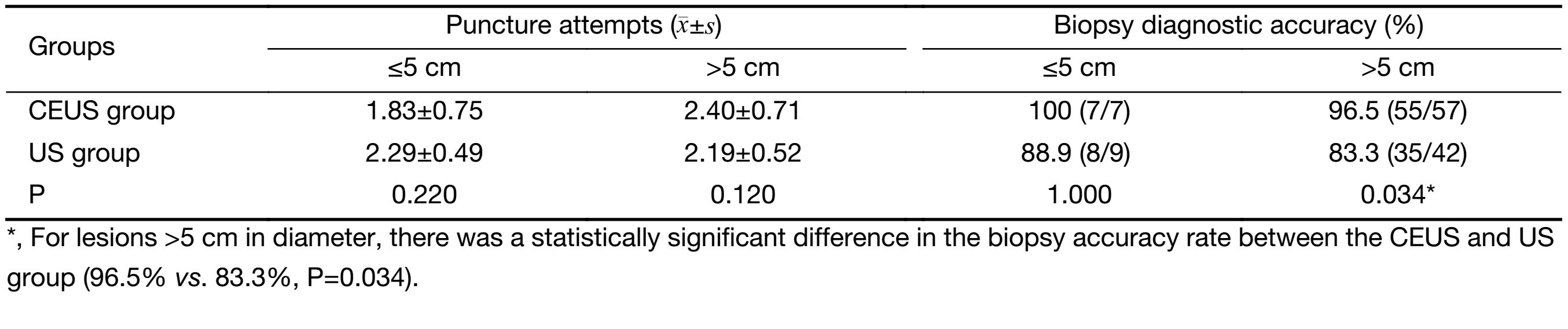
Regarding to the number of biopsy puncture attempts, the CEUS group had a mean of 2.36±0.70 times of puncture attempts, and the US group had 2.21±0.51 times of puncture attempts. The two groups had similar results in the number of puncture attempts (P>0.05, Table 6).
Full table
Using the final diagnosis as the criterion, the biopsy diagnostic accuracy rate was 96.9% (62/64) in the CEUS group, which was significantly higher than 84.3% (43/51) in the US group (P=0.022). We also found the close relationship between tumor sizes and biopsy diagnostic accuracy rates. For lesions ≤5 cm in diameter, the accuracy rates of CEUS group (100%) and US group (88.9%) were not significantly different (P=1.000). For lesions >5 cm in diameter, the accuracy rate of the CEUS group (96.5%) was significantly higher than that of the US group (83.3%, P=0.034, Table 6).
Complications
Two cases in the US group suffered mediastinal hemor- rhage after the needle biopsy (Figure 4). Both patients received hemostasis treatment and prolonged hos-pitalization period. No major complications happened in the CEUS group. Regarding to minor complications, 1 case in the CEUS group and 2 cases in the US group developed slight chest pain after the biopsy and relieved after rest.
Discussion
Mediastinal space-occupying lesions are characterized by complex histological types (13-15). Some lesions lack apparent specific features in both clinical and imaging examinations, therefore, it is difficult to generate a qualitative diagnosis for such lesions. Ultrasound scanning through suprasternal fossa and parasternal intercostal space can reveal most anterior-medial mediastinal lesions. In recent years, ultrasound-guided biopsy has been increasingly applied in the diagnosis of peripheral pulmonary and mediastinal lesions due to its many advantages, such as flexibility, repeatability, non-radiation and real-time monitoring throughout the procedure, compared to chest CT; it can even be performed in general wards (16,17). So the application of ultrasound-guided biopsy technology in mediastinal lesions has attracted increasing attention from clinicians (18).
In general, conventional ultrasound-guided mediastinum biopsy is sufficient to obtain the necessary pathological tissues. However, during the growth process of tumors, tissue liquefaction and necrosis often occur due to inadequate blood supply to the tumors. In addition, most patients lack typical clinical symptoms, which make it difficult to prompt diagnosis, resulting in large lesions. It is relatively difficult to use gray-scale ultrasonography to determine lesion property and whether there is intra-lesion necrosis (19). With the emergence of a new generation of ultrasound contrast agents, such as SonoVue, ultrasound is more convenient than CT scanning to reveal the blood supply inside lesions, because SonoVue is pure blood pool imaging agent (5,20,21). In the present study, we explored the role of CEUS prior to biopsy in mediastinal lesions. CEUS facilitated screening indications for biopsy to avoid zones of liquefied necrosis, thereby achieving a relatively high accuracy rate of biopsy.
CEUS plays a crucial role in the screening of indications for biopsy of solid organs and tissues as well as in guiding biopsy (22-24). Wang et al. and Cao et al. reported that in comparison with conventional ultrasound, CEUS could help to increase the accuracy rate of biopsy of pulmonary peripheral lesions and mediastinal lesions (24,25). However, the report only recruited about 10 patients with mediastinal lesions, which made it difficult for further analyses. Here, we recruited a relatively large sample size of patients undergoing mediastinal biopsy to compare CEUS and conventional ultrasound. We investigated not only the number of needle biopsies, accuracy rate of biopsy, and complications, but also the perfusion feature and neighboring structures of the lesions.
In this study, we performed CEUS-based assessment before biopsy and revealed that 3 cases had large superficial blood vessels in the puncture path, which were difficult to avoid; in addition, another 5 cases had internal necrotic zone being more than 80% of the lesion. Biopsy was therefore not performed for these patients to reduce the false negative rate as well as the risk of complications such as hemorrhage. Biopsy is an invasive diagnostic method and causes pain and complication risk for patients. At this point, CEUS could help to exclude the potential failure cases to avoid unnecessary invasive procedure, which is one of advantage of CEUS application before biopsy.
Ultrasound imaging analysis revealed that compared with the US group, CEUS generated a significantly higher detection rate of internal necrosis as well as a higher accuracy rate of pathological diagnosis for biopsy, which was consistent with the results of Wang et al. (24). Wang et al. performed biopsy of peripheral lung masses and revealed that CEUS improved necrosis detection rate and success rate of biopsy as the lesion size increased compared with conventional ultrasound. Similar to Wang's study, our findings showed that CEUS achieved a statistically significant difference in the display rate of internal necrosis mediastinal lesions, especially the lesions >5 cm in diameter. Hence, using CEUS prior to biopsy for anterior-medial mediastinal lesions could effectively bypass necrotic zones, and select optimal sites of tissue sample. In conventional ultrasound examination, color Doppler was performed to evaluate the vascularity. However, the display of vascularity by color Doppler is not sensitive as CEUS. CEUS could also accurately differentiate the viable regions from necrotic tissues in a lesion. As a consequence, CEUS had super role in screening indications for biopsy and choosing a proper puncture path, compared to color Doppler.
In addition, we also summarized the CEUS feature of lymphoma, thymoma and thymic carcinoma, which commonly occur in anterior-medial mediastinum. The results revealed that lymphoma and thymoma displayed significant differences in enhancement patterns during the arterial phase and thymoma typically manifested homogeneous enhancement. Compared with thymic carcinoma, thymoma had less frequency for internal necrosis. In addition, thymic carcinoma was associated with a significantly higher necrosis rate than that of lymphoma. Comparison of the necrosis rate and pericardial effusion between thymoma and thymic carcinoma before and after CEUS revealed that thymic carcinoma had high accident for internal necrosis and pericardial effusion. This finding could be related with tumor biology that thymic carcinomas are more likely to develop intra-tumor necrosis and pericardium infiltration (26). As a consequence, it provides useful information to distinguish a benign tumor from a malignant tumor.
Moreover, the two groups had no difference in the total number of biopsy attempts. Comparison of the complications revealed that 2 cases in the US group developed mediastinal hemorrhage and prolonged hospitalization period for hemostasis treatment. No patients in the CEUS group developed any severe complications. In both groups, no patients developed other complications, such as pneumothorax, breathing difficulties, or pinhole metastasis (27). This low rate of complication results for biopsy could be explained by our strict screening of indications.
There were some limitations in our study. First, the two groups classified in this study were not randomized. Patients refused CEUS examination mainly because of economic factors. Second, compared to enhanced CT, CEUS has limitation for visualization of mediastinal lesion due to gas or rib. Also CEUS or ultrasound had difficulty to show some small lesions behind the sternum. CEUS-guided biopsy cannot be performed in such cases. Last, although CEUS improved the accuracy rate of biopsy compared to conventional ultrasound, there was high risk for biopsy in lesions close to heart or large vessels. So cautions should be paid in mediastinal biopsy.
Conclusions
In summary, CEUS technique could reliably differentiate the viable regions from necrotic tissues in a lesion and identify large superficial blood vessels in anterior medial mediastinal lesions. As a consequence, this technique may provide valuable information for screening indications for biopsy and choosing a proper puncture path, thereby addressing the shortcomings of conventional ultrasound-guided biopsy. CEUS prior to biopsy could improve the accuracy rate of biopsy, reduce the risk of complications, and thus become clinically important for mediastinal biopsy.
Acknowledgements
Funding: This study was supported by Beijing Municipal Health System Special Funds of High-Level Medical Personnel Construction (No. 2013-3-086), the Natural Science Foundation of Beijing (No. 7152031), and Beijing Baiqianwan Talents Project.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Trinavarat P, Riccabona M. Potential of ultrasound in the pediatric chest. Eur J Radiol 2014;83:1507–18. [PubMed] DOI:10.1016/j.ejrad.2014.04.011
- Nasit JG, Patel M, Parikh B, et al. Anterior mediastinal masses: A study of 50 cases by fine needle aspiration cytology and core needle biopsy as a diagnostic procedure. South Asian J Cancer 2013;2:7–13. [PubMed] DOI:10.4103/2278-330X.105872
- Azrumelashvili T, Mizandari M, Magalashvili D, et al. Imaging guided mediastinal percutaneal core biopsy — technique and complications. Georgian Med News 2015(242):24–34. [PubMed]
- Jeon KN, Bae K, Park MJ, et al. US-guided transthoracic biopsy of peripheral lung lesions: pleural contact length influences diagnostic yield. Acta Radiol 2014;55:295–301. [PubMed] DOI:10.1177/0284185113494984
- Wu W, Chen MH, Yin SS, et al. The role of contrastenhanced sonography of focal liver lesions before percutaneous biopsy. AJR Am J Roentgenol 2006;187:752–61. [PubMed] DOI:10.2214/AJR.05.0535
- Greis C. Quantitative evaluation of microvascular blood flow by contrast-enhanced ultrasound (CEUS). Clin Hemorheol Microcirc 2011;49:137–49. [PubMed] DOI:10.3233/CH-2011-1464
- Jang HJ, Kim TK, Burns PN, et al. CEUS: An essential component in a multimodality approach to small nodules in patients at high-risk for hepatocellular carcinoma. Eur J Radiol 2015;84:1623–35. [PubMed] DOI:10.1016/j.ejrad.2015.05.020
- Yoon SH, Lee KH, Kim SY, et al. Real-time contrastenhanced ultrasound-guided biopsy of focal hepatic lesions not localised on B-mode ultrasound. Eur Radiol 2010;20:2047–56. [PubMed] DOI:10.1007/s00330-010-1757-z
- Sparchez Z, Radu P, Zaharia T, et al. Usefulness of contrast-enhanced ultrasound-guidance in percutaneous biopsies of liver tumors. J Gastrointestin Liver Dis 2011;20:191–6. [PubMed]
- Ewertsen C, Henriksen BM, Torp-Pedersen S, et al. Characterization by biopsy or CEUS of liver lesions guided by image fusion between ultrasonography and CT, PET/CT or MRI. Ultraschall Med 2011;32:191–7. [PubMed] DOI:10.1055/s-0029-1245921
- Wang J, Zhou D, Xie X, et al. Utility of contrastenhanced ultrasound with SonoVue in biopsy of small subpleural nodules. Int J Clin Exp Med 2015;8:15991–8. [PubMed]
- Sartori S, Nielsen I, Trevisani L, et al. Contrastenhanced sonography as guidance for transthoracic biopsy of a peripheral lung lesion with large necrotic areas. J Ultrasound Med 2004;23:133–6. [PubMed]
- Takahashi K, Al-Janabi NJ. Computed tomography and magnetic resonance imaging of mediastinal tumors. J Magn Reson Imaging 2010;32:1325–39. [PubMed] DOI:10.1002/jmri.v32:6
- Araki T, Nishino M, Gao W, et al. Anterior mediastinal masses in the Framingham Heart Study: prevalence and CT image characteristics. Eur J Radiol Open 2015;2:26–31. [PubMed] DOI:10.1016/j.ejro.2014.12.003
- Tomiyama N, Honda O, Tsubamoto M, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol 2009;69:280–8. [PubMed] DOI:10.1016/j.ejrad.2007.10.002
- Diacon AH, Schuurmans MM, Theron J, et al. Safety and yield of ultrasound-assisted transthoracic biopsy performed by pulmonologists. Respir ation 2004;71:519–22. [PubMed] DOI:10.1159/000080638
- Koegelenberg CF, Diacon AH. Pleural controversy: close needle pleural biopsy or thoracoscopy — which first?. Respirology 2011;16:738–46. [PubMed] DOI:10.1111/j.1440-1843.2011.01973.x
- Liao WY, Chen MZ, Chang YL, et al. US-guided transthoracic cutting biopsy for peripheral thoracic lesions less than 3 cm in diameter. Radiology 2000;217:685–91. [PubMed] DOI:10.1148/radiology.217.3.r00dc21685
- Grg C. Transcutaneous contrast-enhanced sonography of pleural-based pulmonary lesions. Eur J Radiol 2007;64:213–21. [PubMed] DOI:10.1016/j.ejrad.2007.06.037
- Kong WT, Wang WP, Cai H, et al. The analysis of enhancement pattern of hepatic inflammatory pseudotumor on contrast-enhanced ultrasound. Abdom Imaging 2014;39:168–74. [PubMed] DOI:10.1007/s00261-013-0051-3
- Wang JW, Zheng W, Chen Y, et al. Quantitative assessment of tumor blood flow changes in a murine breast cancer model after adriamycin chemotherapy using contrast-enhanced destruction-replenishment sonography. J Ultrasound Med 2013;32:683–90. [PubMed]
- Nasr P, Hilliges A, Thorelius L, et al. Contrastenhanced ultrasonography could be a non-invasive method for differentiating none or mild from severe fibrosis in patients with biopsy proven non-alcoholic fatty liver disease. Scand J Gastroenterol 2016;51:1126–32. [PubMed] DOI:10.3109/00365521.2016.1172336
- Coran A, Di Maggio A, Rastrelli M, et al. Core needle biopsy of soft tissue tumors, CEUS vs US guided: a pilot study. J Ultrasound 2015;18:335–42. [PubMed] DOI:10.1007/s40477-015-0161-6
- Wang S, Yang W, Zhang H, et al. The role of contrast-enhanced ultrasound in selection indication and improveing diagnosis for transthoracic biopsy in peripheral pulmonary and mediastinal lesions. Biomed Res Int 2015;2015:231782. [PubMed] DOI:10.1155/2015/231782
- Cao BS, Wu JH, Li XL, et al. Sonographically guided transthoracic biopsy of peripheral lung and mediastinal lesions: role of contrast-enhanced sonography. J Ultrasound Med 2011;30:1479–90. [PubMed]
- Wu J, Fang W, Chen G. The enlightenments from ITMIG Consensus on WHO histological classification of thymoma and thymic carcinoma: refined definitions, histological criteria, and reporting. J Thorac Dis 2016;8:738–43. [PubMed] DOI:10.21037/jtd
- Fang WT, Xu MY, Chen G, et al. Minimally invasive approaches for histological diagnosis of anterior mediastinal masses. Chin Med J (Engl) 2007;120:675–9. [PubMed]