Health-related quality of life among rural residents aged 45−69 years in Hua County, Henan Province, China: Results of ESECC Trial for esophageal cancer screening with endoscopy
Introduction
With the socio-economic development, the biomedical model has undergone change to a biopsychosocial model (1). Traditional health indicators, such as morbidity, mortality and survival do not fully reflect overall health status (2). Health related quality of life (HRQOL) refers to the overall impact of physical, mental, and social well-being on an individual, and reflects mainly on the individual’s life itself rather than on the length of survival (3). This has been increasingly recognized to be an endpoint which can serve to measure health needs (4).
China is an agricultural country with 1.3 billion people and 70% of Chinese people live in rural areas (5). There is an obvious gap between the levels of urban and rural health, and the health level of rural residents is still relatively low (5). In 2016 the Chinese central government proposed the “The Thirteenth Five-Year Plan” and improving life quality and eliminating poverty in rural areas is one of the major goals of this plan (6). There has been a growing acceptance of the need for understanding the current status of the life quality and risk factors in rural populations, which can help to establish and regulate relevant health policy and effectively eliminate factors which adversely impact health equity between rural and urban populations, and thus improve the overall level of health for rural Chinese people.
Unfortunately, there have been few population-based studies evaluating HRQOL in rural populations in China, and defects in study design of most previous studies such as inadequate sample size, flawed sampling sources and statistical analysis (7,8) have limited the reliability of the conclusions and the comparability among studies. Moreover, these studies focused predominantly on exploring the association of socio-economic status and HRQOL, which is insufficient for fully understanding the risk factors which may impact HRQOL.
In this study, we investigated current HRQOL findings in over 12,000 rural adults aged 45–69 years, and explored risk factors for low HRQOL on the basis of a large randomized trial in rural Hua County, Henan Province, China (9). The goal of this study was to identify the vulnerabilities and principal risk factors which impact life quality in this population, and to provide intervention targets for health promotion programs in rural China.
Materials and methods
Study subjects
Hua County of Henan Province, with a rural population of 1.1 million, is an agricultural region in northern part of China, and the per capita GDP was $2,430 in 2013 (10). The mortality for esophageal squamous cell carcinoma (ESCC) in this area is among the highest in the world (9).
In January 2012, we initiated the Endoscopic Screening for Esophageal Cancer in China (ESECC) randomized controlled trial (ClinicalTrials.gov identifier: NCT01688908) in Hua County to evaluate the efficacy and cost-effectiveness of population level endoscopic screening for ESCC. The inclusion criteria in the ESECC trial were: 1) permanent residency in a target village; 2) age 45–69 years (with >5 years of life expectancy) and no history of endoscopic examination within 5 years prior to the initial interview; 3) no history of cancer or mental disorder; 4) negative for hepatitis B virus, hepatitis C virus and human immunodeficiency virus; and 5) agreement to complete all phases of the trial ( 9).
Based on the ESECC trial, from November 2015 to September 2016, we interviewed 12,085 residents from 257 target villages with total population sizes ranging from 500 to 3,000 which were randomly selected from 18 towns in Hua county.
EQ-5D instrument
The EQ-5D-3L was developed as a standardized non-disease-specific measure of HRQOL by the EuroQoL Group, a voluntary multinational collaboration of European investigators (11). This instrument consists of five dimensions, mobility, self-care, usual activities, pain/discomfort and anxiety/depression. Each dimension has three levels of severity ranked as no problem, some/moderate problems, and severe/extreme problems (coded 1, 2 and 3 respectively). For example, state 11111 represents full health (no problems on any dimension), whereas state 33333 represents an extreme problem on all five dimensions. The EQ-5D-3L has 245 kinds of health conditions, including “unconscious” and “death” which are considered as health states.
In practical terms, the EQ-5D-3L has the advantage of being a simple instrument, which is easy to use with good response rates, so it has been one of the most commonly applied generic HRQOL instruments, particularly in less-educated elderly population (12). The validity and reliability of the EQ-5D-3L scale have been tested in China (13).
HRQOL results measured by the EQ-5D-3L were converted to index scores (health utility scores) using the China time trade-off value sets (ranging from –0.149 for the worst health status to 1.00 representing the best health rating) which were developed by Liu et al. in 2014 (14).
Questionnaire investigation
A computer aided one-on-one questionnaire was also completed by all participants in the interview to investigate potential risk factors associated with low HRQOL, which included demographic factors (age, gender), socio-economic status (educational level, job type, household annual per capita income), household factors (living arrangement, source of drinking water, family members smoking), behavioral and mental factors (cigarette smoking, alcohol drinking, testiness), dietary habits (regularity of eating, eating speed, dietary pattern) and health status [body mass index (BMI), upper gastrointestinal cancer related symptoms, chronic diseases] (Supplementary File S1).
Statistical analysis
We transformed the continuous EQ-5D-3L index scores into binary variable and respondents who were below the tenth percentile of index scores were defined as having a poor quality of life (coded 1), others were good (coded 0). In addition, due to the ceiling effects of EQ-5D-3L (15), we regrouped the three response levels (no problem, some/moderate problems and extreme problems) into two categories, namely no problem and any problem (coded 0 and 1, respectively).
All variables were first evaluated with unconditional univariate logistic regression analysis. Age, gender and variables with P<0.05 were subjected to multivariate logistic regression model analysis and backward selection with P<0.05 was used to explore potential risk factors for low quality of life. Odds ratio (OR) and 95% confidence interval (95% CI) were estimated taking village cluster into account (16), and pairwise interactions were exhaustively tested in multivariate models. Due to rigorous logic checking of our computer-based investigation system, there were few missing data in this study. The living arrangement information and body mass index (BMI) were not available in 3 (0.02%) and 41 (0.34%) subjects respectively, and they were excluded from the regression analysis. There were 1,002 (8.29%) respondents who refused to declare their income, so we conducted sensitive analysis by including and not including the household annual per capita income variable in the multivariate logistic regression analysis. As the results were similar, only results from the analysis based on the models not including the household annual per capita income variable were presented.
All statistical analysis was performed using STATA (Version 13.1; StataCorp LLC, TX, USA). All tests were two-sided and had a significance level of 0.05.
Ethics statement
Research protocols were approved by the Institutional Review Board of Peking University Cancer Hospital, Beijing, China. All participants provided written informed consent before the survey.
Results
Proportion of full health by selected sociodemographic and health characteristics
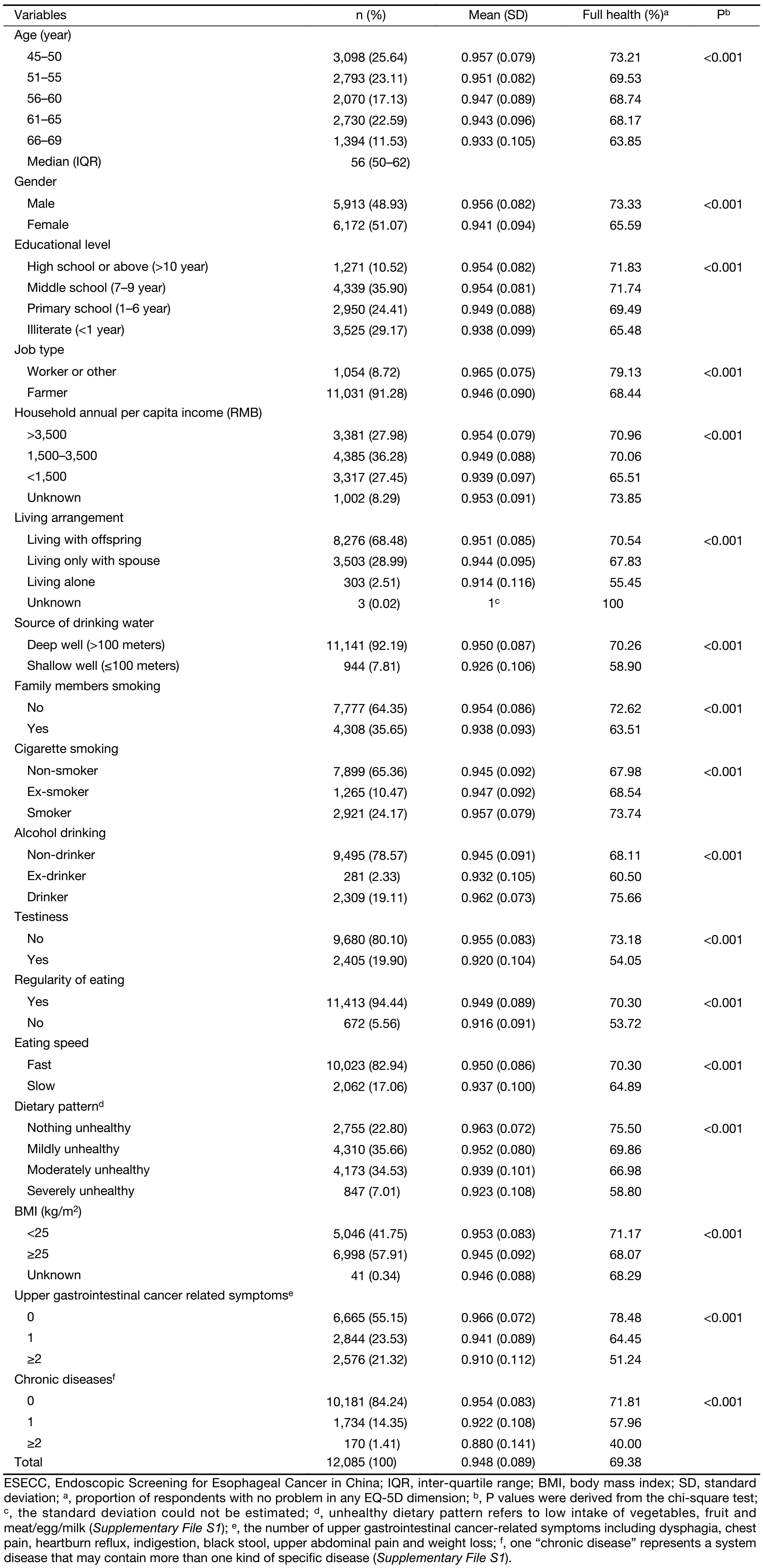
From 2015 to 2016, a total of 12,085 permanent residents (median age 56 years; male-female ratio 0.96) from rural Hua County were interviewed. Selected demographic and behavioral characteristics of the participants are shown in Table 1. All respondents were of Han ethnicity and 91.28% of the respondents were farmers. The respondents had an average EQ-5D-3L index score of 0.948 (standard deviation=0.089), and 69.38% of the respondents reported full health status. The proportion of full health varied with the demographic and behavioral characteristics of the participants. Older age, female gender, lower educational level, farming as occupation, lower levels of household annual per capita income, living alone, using shallow wells as main source of drinking water, exposure to family members smoking, testiness, irregular eating, eating slowly, unhealthy dietary pattern, overweight or obesity, upper gastrointestinal cancer related symptoms and chronic diseases were associated with a lower proportion of full health (P<0.001). In addition, smokers and drinkers had a higher proportion of full health than who did not smoke or drink (P<0.001).
Full table
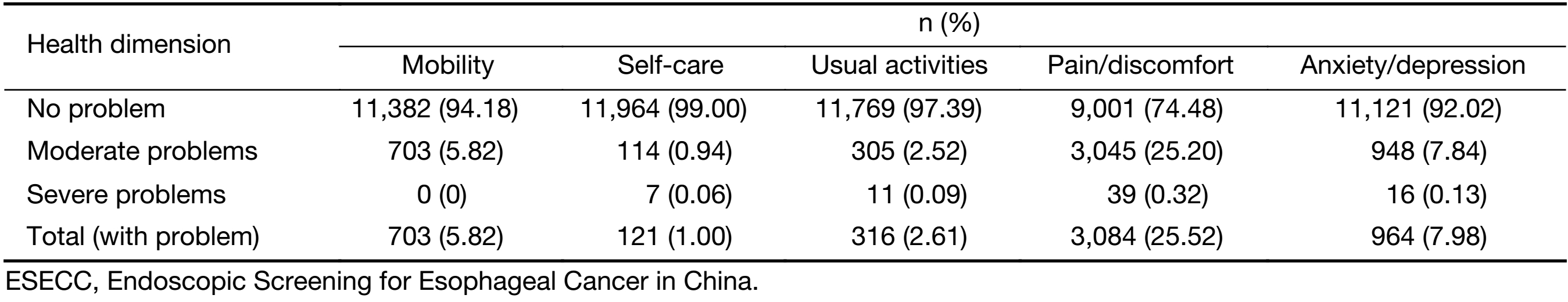
Health status distribution in five dimensions of EQ-5D
Among the five dimensions under evaluation, pain/discomfort was the most frequently reported problem (25.52%, 95% CI: 24.75%–26.30%), followed by anxiety/depression (7.98%, 95% CI: 7.51%–8.47%), mobility (5.82%, 95% CI: 5.41%–6.25%), usual activities (2.61%, 95% CI: 2.34%–2.91%) and self-care (1.00%, 95% CI: 0.84%–1.20%). The prevalence of severe problems in all dimensions was less than 0.50% (Supplementary Table S1).
HRQOL by age and gender
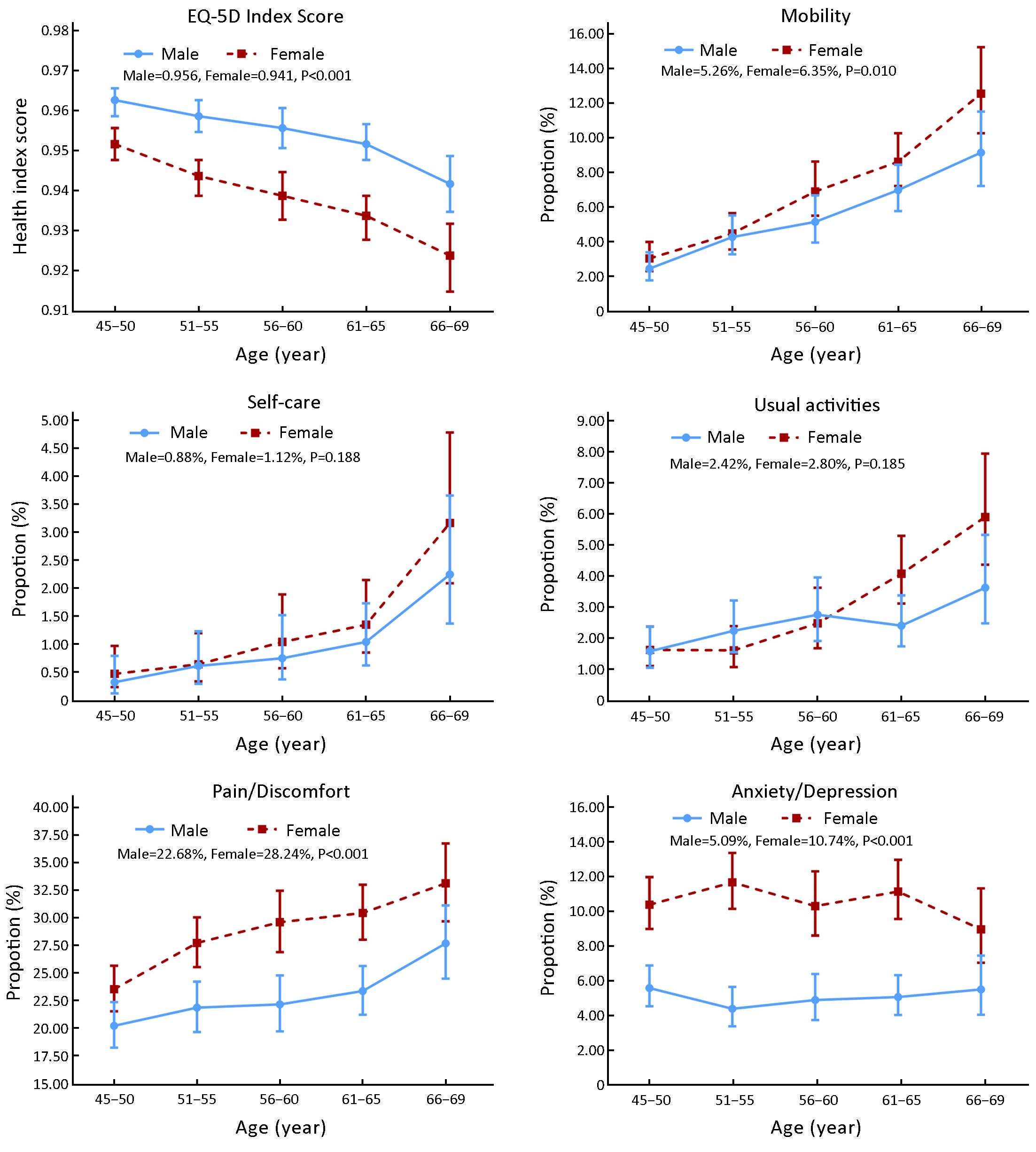
As shown in Figure 1, the total EQ-5D index score decreased with age in both males and females, and men had a higher mean score than women in all age groups (0.956 vs. 0.941, P<0.001). The proportion of participants with EQ-5D identified problems increased with age in all dimensions except for the anxiety/depression dimension. Women tended to have more problems than men with mobility (P=0.01), pain/discomfort (P<0.001) and anxiety/depression (P<0.001). Although men and women had no differences in usual activities on the whole (P=0.185), we found that women had a significantly higher proportion of reported activity related problems than men after 55 years old (P<0.001).
Risk factors for HRQOL
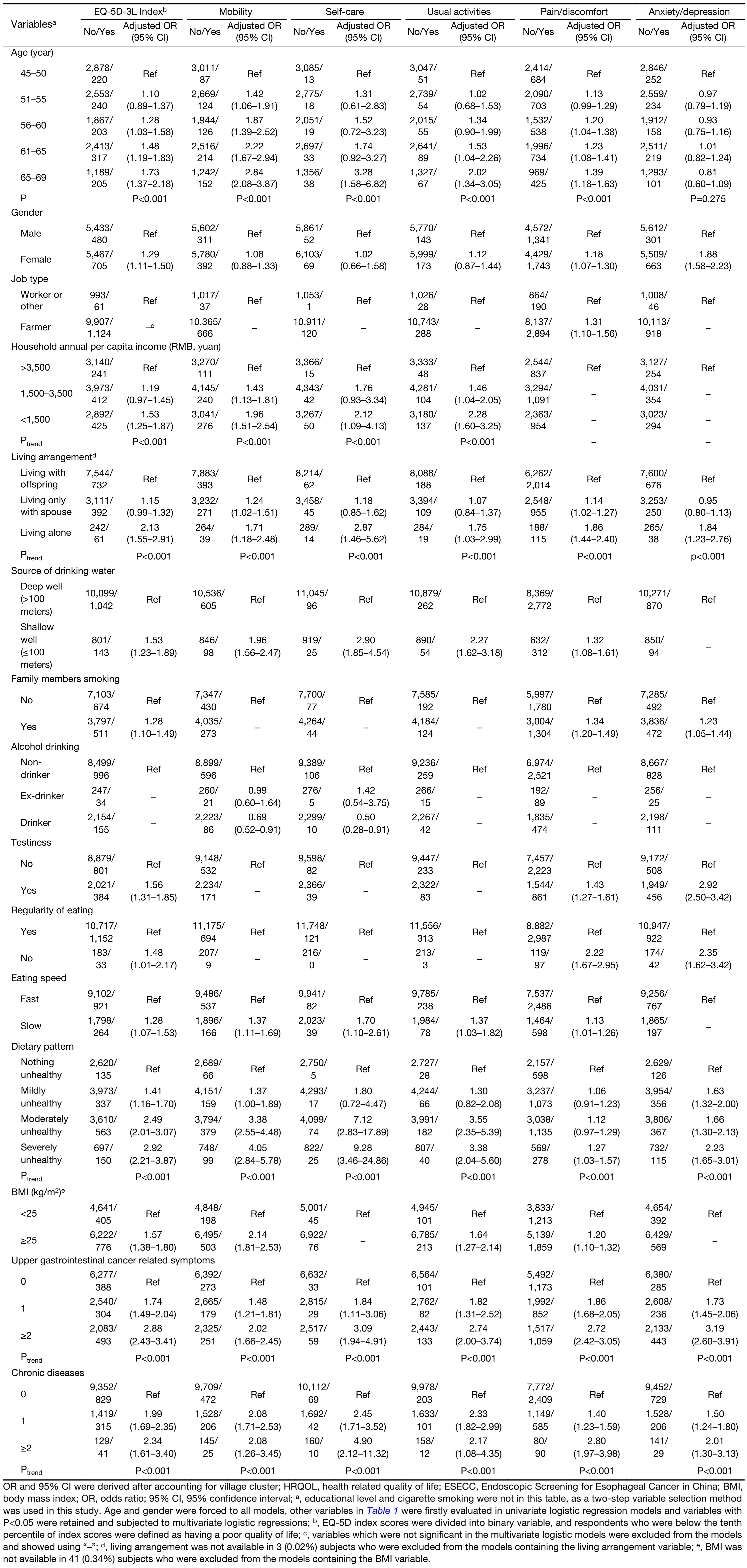
As shown in Table 2 and Supplementary Table S2, lower EQ-5D-3L index scores were associated with older age (Ptrend<0.001), female gender (OR=1.29, 95% CI: 1.11–1.50), lower levels of household annual per capita income (Ptrend<0.001), living alone (Ptrend<0.001), using shallow wells as main source of drinking water (OR=1.53, 95% CI: 1.23–1.89), exposure to family members smoking (OR=1.28, 95% CI: 1.10–1.49), testiness (OR=1.56, 95% CI: 1.31–1.85), irregular eating (OR=1.48, 95% CI: 1.01–2.17), eating slowly (OR=1.28, 95% CI: 1.07–1.53), unhealthy dietary pattern (Ptrend<0.001), overweight or obesity (OR=1.57, 95% CI: 1.38–1.80), upper gastrointestinal cancer related symptoms (Ptrend<0.001) and chronic diseases (Ptrend<0.001). Among these factors, living alone, unhealthy dietary pattern, upper gastrointestinal cancer related symptoms and chronic diseases had a significantly negative impact on all of the five dimensions which were evaluated. Although job type and alcohol drinking did not impact the overall HRQOL, respondents who engaged in farming reported more problems with pain/discomfort, and alcohol drinking had slight protective effects in mobility and self-care dimensions.
Full table
Interaction evaluation
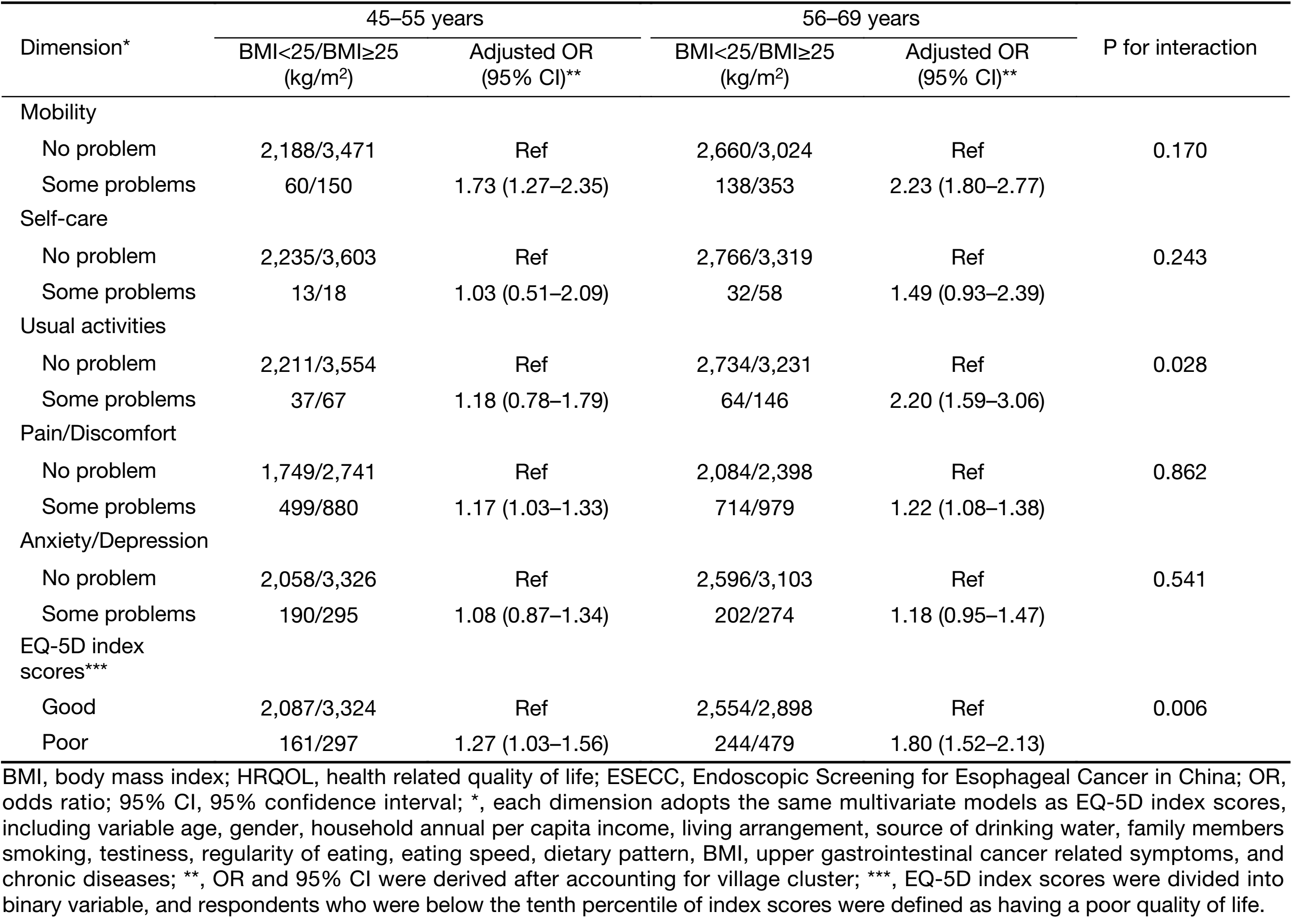
As is shown in Table 3, we found the modification effect of age on the relationship between BMI and quality of life. Overweight or obese subjects had a significantly higher risk of low quality of life in the 56–69 year group than in the 45–55 year group (OR56–69y=1.80, OR45–55y=1.27, Pinteraction=0.006), which was mainly resulted from the usual activities dimension (OR56–69y=2.20, OR45–55y=1.18, Pinteraction=0.028).
Full table
Discussion
In this cross-sectional study, we investigated 12,085 rural residents aged 45–69 years from Hua County and found that up to 30.62% reported problems in at least one EQ-5D dimension. A series of risk factors for low quality of life in this rural population were also evaluated. This is the first population-based study using random sampling to evaluate the HRQOL status and risk factors which impact HRQOL in a rural population in China.
Pain/discomfort and anxiety/depression were the most commonly reported dimensions with moderate or severe health problems, which is consistent with previous studies from other regions of China (5,7,17). International studies among general populations aged 60 years and older from Asia (18) and Europe (19,20) also identified pain/discomfort as the most common problem with a prevalence ranging of 29.4%–61.3%. Thus, relieving of physical discomfort should be a global priority in prevention of HRQOL deterioration in community level health care programs.
The mean EQ-5D index score in this population was 0.948, which is lower than the scores reported in two previous studies of urban populations in China using the same health utility weights for calculating health index scores. A community based study in Suzhou, which is an urban metropolis in East China, investigated 5,557 inhabitants aged 60 years and older and reported a mean EQ-5D index score of 0.959 (17). For purposes of comparison, we also calculated the health index score in our rural population of individuals aged 60–69 years, and the mean score was 0.941. Another cross-sectional survey in 13 provinces across China from 2013 to 2014 which was a part of the Cancer Screening Program in Urban China (CanSPUC) reported that the mean EQ-5D index score was 0.96 for 11,699 participants with an age range similar to participants in our study (21). The urban-rural health inequality in China has been reported to be associated not only with natural conditions and socio-economic development, but also with allocation of health care resources and health services (5). The quality and accessibility of primary health care services play an important role in the health of the population in rural Chinese areas, and these factors should be targets of the health promotion programs to eliminate the urban-rural disparities in the overall quality of life.
We found that the EQ-5D index scores decreased with age, and women reported lower quality of life than men. This was also consistent with previous studies both from China (7,17) and other countries (18-20). Older people were more likely to experience problems in the physical domains of EQ-5D than their younger counterparts in this study. This finding may further serve to explain that more severe disabilities in activity, cognitive impairment and poor physical functioning may be the main causes of poor quality of life among the elderly (17,22). Lower quality of life among women was mainly due to problems with pain/discomfort and anxiety/depression in this study. Possible explanations for this gender difference are as follows. First, women may be more sensitive to pain and other physical discomfort than men (23). Second, women in Asia-pacific countries are more vulnerable to the conditions of lower socio-economic status including fewer job opportunities, lower wages and discriminatory attitudes and so on (24), which may lead to negative psychologic pressure.
People living alone had the poorest quality of life than those living with their offspring or spouse in this rural population. Studies from Japan (25), the UK (26) and the US (27) also reported that living alone was significantly and negatively correlated with mental health, life satisfaction and self-rated health among the elderly. Similarly, China’s 4th National Household Health Survey in 2008 reported that Chinese urban elders who lived with their offspring or spouse had better HRQOL than those living alone (28). Lack of financial and social support, companionship and daily care from family members may be principal reasons. In addition, we found that the elderly living only with spouse reported more physical problems than those living with their offspring. The explanation for this finding may be economic independence. The majority of rural residents in China do not have unemployment insurance or retirement pension, and their social and health security is dependent largely on their family, particularly their offspring. There has been an increasing trend of migration among the young labor force from rural to urban areas because of urbanization in China (29), which may leave more and more elderly people living on their own with less physical and emotional support. Strengthening the social support system and basic medical services among the rural elderly is likely to be measures for improving their quality of life.
Water source has not been a commonly reported factor which impacts HRQOL, especially in developed countries. Since the 1980’s, the Chinese government has committed significant resources to an extensive water improvement project, and deep groundwater (>100 meters) has become the main water source for most of the inhabitants of rural Hua county (30). We found that 7.81% of the residents who still used shallow wells as main water source had a lower quality of life and more problems in physical health than those who did not. A previous cross-sectional survey in mid-east rural China also reported that the quality of a water source (deep groundwater or public water system vs. surface or shallow well water) was positively associated with the HRQOL score (31). The shallow ground water source was more likely to result in exposure to chemical and biological pollution (32), which may be potential risk factors to physical health, and thus lead to a decline in quality of life. From a more macroscopic perspective, the quality of a water source may reflect the individual’s level of socio-economic status, which is also a crucial determinant of life quality (33).
Obesity, which is a clear risk factor for physical health, also leads to a decrease in the physical domain of HRQOL in our study, especially in individuals of 55 years or older. The obesity epidemic in low-income and middle-income countries is mainly a result of unhealthy dietary habits and physical inactivity (34). This low-income, less-educated population tended to use low-protein high-energy pasta as main dietary staple, and at the same time poor social resources limited their chances of physical activity. Comprehensive life style intervention for weight control and improvement of physical fitness such as dietary education and establishment of physical exercise facilities would likely play an important role for improvement of quality of life in this rural population, especially for older people.
Cancer has become a major public health problem in China since 2010 (35). The ESCC incidence and mortality vary by economic level and geographic location, which have brought about extremely heavy burden to the “high-risk” regions (36,37). We found that esophageal cancer related symptoms had a stable negative impact on life quality in this high prevalence population for ESCC, which suggested that physical symptoms due to the high-prevalence disease might lead to the decline of general quality of life. We found that chronic diseases, which are worldwide risk factors for quality of life in the elderly (38), were also strongly associated with low HRQOL in this population, and this further demonstrated that primary health care services and chronic disease management are crucial for improving the overall health status in this rural population.
This study has two limitations that should be acknowledged. First, we could not conclude a causal relationship between these factors and HRQOL due to the nature of cross-sectional investigation. Second, although high-grade sampling method was adopted, respondents of this study were restricted to those from Hua County, Henan Province, which might limit the generalizability of our findings to other rural population in China.
Conclusions
This large population-based survey reports the current HRQOL status and describes a series of risk factors which impact HRQOL in this rural population in China using random sampling methodology. The overall quality of life among Chinese rural residents was relatively low by objective measurement. Health intervention and promotion programs in rural China are needed, and more attention should be given to the elderly, especially to elderly women and the elderly living alone. Alleviation of poverty, improvement of basic living conditions and primary medical care should be priorities for improvement of the overall HRQOL in rural China. Results of this study are crucial for generating health promotion strategy in rural population in China, and will also serve as the fundamental basis for the cost-utility evaluation in our ESECC screening trial in the future.
Acknowledgements
This work was supported by the Charity Project of National Ministry of Health (No. 201202014), the Natural Science Foundation of China (No. 81473033), the National Key R&D Program of China (No. 2016YFC0901404), the Science Foundation of Peking University Cancer Hospital (No. 2017-4) and the Open Project funded by Key Laboratory of Carcinogenesis and Translational Research, Ministry of Education/Beijing (No. 2017-10).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Supplementary File S1
Information regarding definitions and coding forms of potential risk factors investigated in this study
Age
Age at enrollment was calculated as 
Cigarette smoking and alcohol drinking
Participants were asked about their life-time smoking and alcohol drinking history. Cigarette smoking was defined as a smoking history of at least 18 packs over 1 year, and alcohol drinking was defined as drinking Chinese liquor (containing >40% alcohol) at least twice a week for ≥12 months (consumption of other kinds of alcoholic beverages such as beer and wine is very rare in the study area). In this study, the smoking and drinking status (coded as 0 or 1) of each participant was used in the analysis.
Testiness
Participants were asked about whether they are prone to be testy? This question had two options: 1) no; and 2) yes. Subjects selecting 1) were coded as 0 and those selecting 2) were coded as 1.
Family members smoking
Participants were asked about whether they live with any family members who smoke. This question had two options: 1) no; and 2) yes. Subjects selecting 1) were coded as 0 and those selecting 2) were coded as 1.
Source of drinking water
This question had two options: 1) deep well; and 2) shallow well. Subjects selecting 1) were coded as 0 and those selecting 2) were coded as 1. Deep well water was defined as motor-pumped groundwater from a depth of ≥100 meters.
Dietary habits
Five questions about dietary habits were asked as follows:
1. Regularity of eating
This question had three options: 1) habitually eating regularly; 2) sometimes eating regularly; and 3) eating irregularly.
Subjects selecting 1) and 2) were coded as 0 and those selecting 3) were coded as 1.
2. Eating speed
This question had three options: 1) slow; 2) sometimes fast; and 3) always fast. Subjects selecting 2) and 3) were coded as 0 and those selecting 1) were coded as 1.
3. Unhealthy dietary pattern
Participants were asked with three questions about their intake of vegetable, fruit and meat/egg/milk. Each question had three options: 1) no (<1 times per week); 2) sometimes (1−3 times per week); and 3) frequently (≥4 times per week). Subjects selecting 3) in three, two, one and none of all the questions were defined as nothing, mildly, moderately, and severely unhealthy dietary pattern, which were coded as 0, 1, 2 and 3 respectively in this study.
Body mass index (BMI)
BMI was calculated as body weight in kilograms divided by the square of body height in meters (kg/m2). Subjects were categorized into two groups as BMI <25 (coded as 0) and BMI ≥25 (coded as 1) according to the overweight standard of World Health Organization (WHO).
Upper gastrointestinal cancer related symptoms
Seven questions regarding upper gastrointestinal cancer related symptoms were asked as follows: unexplained dyspepsia, chest pain, heartburn reflux, indigestion, black stool, upper abdominal pain and weight loss. Each question had three options: 1) no (<1 times per week); 2) sometimes (1–3 times per week); and 3) frequently (≥4 times per week). Subjects selecting 1) were coded as 0 and those selecting 2) and 3) were coded as 1. The number of these symptoms was counted for each participant and was evaluated in the logistic regression models.
Chronic diseases
All reported chronic diseases were classified as digestive, respiratory, cardiocerebral, vascular, endocrine, motor and urinary system diseases according to the international Classification of diseases (ICD-10). One “chronic disease” in the statistical analysis represents a system disease that may contain more than one kind of specific disease. The number of system diseases was counted for each participant and was evaluated in the logistic regression models.
Full table

Full table
References
- Engel GL. Sounding board. The biopsychosocial model and medical education. Who are to be the teachers?. N Engl J Med 1982;306:802–5. [PubMed] DOI:10.1056/NEJM198204013061311
- Collins B. Using a survey to estimate health expectancy and quality-adjusted life expectancy to assess inequalities in health and quality of life. Value Health 2013;16:599–603. [PubMed] DOI:10.1016/j.jval.2013.01.004
- Bowling A. The concept of quality of life in relation to health. Med Secoli 1995;7:633–45. [PubMed]
- Varni JW, Burwinkle TM, Lane MM. Health-related quality of life measurement in pediatric clinical practice: an appraisal and precept for future research and application. Health Qual Life Outcomes 2005;3:34. [PubMed] DOI:10.1186/1477-7525-3-34
- Sun S, Chen J, Johannesson M, et al. Regional differences in health status in China: population health-related quality of life results from the National Health Services Survey 2008. Health Place 2011;17:671–80. [PubMed] DOI:10.1016/j.healthplace.2011.01.007
- National Development and Reform Commission. Guide to the Thirteenth Five-Year Plan of Henan Province. Available online: http://ghs.ndrc.gov.cn/ghwb/dfztgh/201606/P020160617604395628110.pdf
- Zhang T, Shi W, Huang Z, et al. Influence of culture, residential segregation and socioeconomic development on rural elderly health-related quality of life in Guangxi, China. Health Qual Life Outcomes 2016;14:98. [PubMed] DOI:10.1186/s12955-016-0499-2
- Li H, Wei X, Ma A, et al. Inequalities in health status among rural residents: EQ-5D findings from household survey China. Int J Equity Health 2014;13:41. [PubMed] DOI:10.1186/1475-9276-13-41
- Liu M, Liu Z, Cai H, et al. A model to identify individuals at high risk for esophageal squamous cell carcinoma and precancerous lesions in regions of high prevalence in China. Clin Gastroenterol Hepatol 2017;15:1538–46. [PubMed] DOI:10.1016/j.cgh.2017.03.019
- Li X, Cai H, Wang C, et al. Economic burden of gastrointestinal cancer under the protection of the New Rural Cooperative Medical Scheme in a region of rural China with high incidence of oesophageal cancer: cross-sectional survey. Trop Med Int Health 2016;21:907–16. [PubMed] DOI:10.1111/tmi.12715
- EuroQol Group. EuroQol — a new facility for the measurement of health-related quality of life. Health Policy 1990;16:199–208. [PubMed]
- Holland R, Smith RD, Harvey I, et al. Assessing quality of life in the elderly: a direct comparison of the EQ-5D and AQoL. Health Econ 2004;13:793–805. [PubMed] DOI:10.1002/hec.858
- Wang HM, Patrick DL, Edwards TC, et al. Validation of the EQ-5D in a general population sample in urban China. Qual Life Res 2012;21:155–60. [PubMed] DOI:10.1007/s11136-011-9915-6
- Liu GG, Wu H, Li M, et al. Chinese time trade-off values for EQ-5D health states. Value Health 2014;17:597–604. [PubMed] DOI:10.1016/j.jval.2014.05.007
- Feng Y, Devlin N, Herdman M. Assessing the health of the general population in England: how do the three- and five-level versions of EQ-5D compare?. Health Qual Life Outcomes 2015;13:171. [PubMed] DOI:10.1186/s12955-015-0356-8
- de Souza RJ, Eisen RB, Perera S, et al. Best (but oft-forgotten) practices: sensitivity analyses in randomized controlled trials. Am J Clin Nutr 2016;103:5–17. [PubMed] DOI:10.3945/ajcn.115.121848
- Pan CW, Wang X, Ma Q, et al. Cognitive dysfunction and health-related quality of life among older Chinese. Sci Rep 2015;5:17301. [PubMed] DOI:10.1038/srep17301
- Hoi le V, Chuc NT, Lindholm L. Health-related quality of life, and its determinants, among older people in rural Vietnam. BMC Public Health 2010;10:549. [PubMed] DOI:10.1186/1471-2458-10-549
- Mangen MJ, Bolkenbaas M, Huijts SM, et al. Quality of life in community-dwelling Dutch elderly measured by EQ-5D-3L. Health Qual Life Outcomes 2017;15:3. [PubMed] DOI:10.1186/s12955-016-0577-5
- Luthy C, Cedraschi C, Allaz AF, et al. Health status and quality of life: results from a national survey in a community-dwelling sample of elderly people. Qual Life Res 2015;24:1687–96. [PubMed] DOI:10.1007/s11136-014-0894-2
- Shi JF, Huang HY, Guo LW, et al. Quality-of-life and health utility scores for common cancers in China: a multicentre cross-sectional survey. Lancet 2016;388(Suppl 1):S29. DOI:10.1016/S0140-6736(16)31956-0>
- Zeng Y, Feng Q, Hesketh T, et al. Survival, disabilities in activities of daily living, and physical and cognitive functioning among the oldest-old in China: a cohort study. Lancet 2017;389:1619–29. [PubMed] DOI:10.1016/S0140-6736(17)30548-2
- Greenspan JD, Craft RM, LeResche L, et al. Studying sex and gender differences in pain and analgesia: a consensus report. Pain 2007;132(Suppl 1):S26–45. [PubMed] DOI:10.1016/j.pain.2007.10.014
- Low WY, Binns C. Gender Issues and Public Health. Asia Pac J Public Health 2016;28:104–6. [PubMed] DOI:10.1177/1010539516637705
- Togari T, Yokoyama Y. Application of the eight-item modified medical outcomes study social support survey in Japan: a national representative cross-sectional study. Qual Life Res 2016;25:1151–8. [PubMed] DOI:10.1007/s11136-015-1155-8
- Hawton A, Green C, Dickens AP, et al. The impact of social isolation on the health status and health-related quality of life of older people. Qual Life Res 2011;20:57–67. [PubMed] DOI:10.1007/s11136-010-9717-2
- Pinillos-Patiño Y, Prieto-Suárez E, Herazo-Beltrán Y. Elderly people’s level of participation in social and recreational activities in Barranquilla, Colombia. Rev Salud Publica (Bogota) (in Spanish) 2013;15:850–7. [PubMed]
- Sun X, Lucas H, Meng Q, et al. Associations between living arrangements and health related quality of life of urban elderly people: a study from China. Qual Life Res 2011;20:359–69. [PubMed] DOI:10.1007/s11136-010-9752-z
- Gong P, Liang S, Carlton EJ, et al. Urbanisation and health in China. Lancet 2012;379:843–52. [PubMed] DOI:10.1016/S0140-6736(11)61878-3
- He Z, Zhao Y, Guo C, et al. Prevalence and risk factors for esophageal squamous cell cancer and precursor lesions in Anyang, China: a population-based endoscopic survey. Br J Cancer 2010;103:1085–8. [PubMed] DOI:10.1038/sj.bjc.6605843
- Zhou J, Ru X, Hearst N. Individual and household-level predictors of health related quality of life among middle-aged people in rural Mid-east China: a cross-sectional study. BMC Public Health 2014;14:660. [PubMed] DOI:10.1186/1471-2458-14-660
- Wu C, Luo Y, Gui T, et al. Concentrations and potential health hazards of organochlorine pesticides in (shallow) groundwater of Taihu Lake region, China. Sci Total Environ 2014;470-1:1047–55. [PubMed] DOI:10.1016/j.scitotenv.2013.10.056
- Sun S, Chen J, Johannesson M, et al. Regional differences in health status in China: population health-related quality of life results from the National Health Services Survey 2008. Health Place 2011;17:671–80. [PubMed] DOI:10.1016/j.healthplace.2011.01.007
- Cecchini M, Sassi F, Lauer JA, et al. Tackling of unhealthy diets, physical inactivity, and obesity: health effects and cost-effectiveness. Lancet 2010;376:1775–84. [PubMed] DOI:10.1016/S0140-6736(10)61514-0
- Lan L, Cai Y, Zhang T, et al. Influencing factors of inpatient expenditure pattern for cancer in China, 2015. Chin J Cancer Res 2017;29:11–7. [PubMed] DOI:10.21147/j.issn.1000-9604.2017.01.02
- Yang Z, Zheng R, Zhang S, et al. Comparison of cancer incidence and mortality in three GDP per capita levels in China, 2013. Chin J Cancer Res 2017;29:385–94. [PubMed] DOI:10.21147/j.issn.1000-9604.2017.05.02
- Chen W, Zheng R, Zhang S, et al. Cancer incidence and mortality in China in 2013: an analysis based on urbanization level. Chin J Cancer Res 2017;29:1–10. [PubMed] DOI:10.21147/j.issn.1000-9604.2017.01.01
- Prince MJ, Wu F, Guo Y, et al. The burden of disease in older people and implications for health policy and practice. Lancet 2015;385:549–62. [PubMed] DOI:10.1016/S0140-6736(14)61347-7
